Although evidence-based medicine (EBM) is now formally referred to as the standard of medical care delivery, there are substantial concerns over its weaknesses and lack of utility on several levels.
For one, it transforms the complex process of clinical decision making that includes years of medical knowledge, experience, and data gathering into an algorithmic exercise that is not individualized for specific clinical scenarios and therefore subject to error in patient care. This algorithmic recommendation is based on the use of randomized control trials (RCTs) and systematic review/meta-analysis as the “gold standard”. But RCTs and review analysis are simply a comparison of one treatment to another, not some superior form of truth.
In relying on these epidemiological tools, EBM does not incorporate the “soft” data that clinicians use to formulate diagnoses and treatments. These “soft” data are many and incorporate a wide range, from the address of the patient, cultural background, family situation, time of the year, and educational background, to how the person talks, who is accompanied by the patient, or even what day of the week the patient is being seen, and these are just a few.
These “soft” data are the basis of the practice of medicine called “Custom-Based Medicine,” where each patient is assessed individually and his or her management shaped accordingly. It is true that Calvin Klein and Armani suits and dresses are great when presented by a very sophisticated model, but their different standard sizes cannot fit every individual. A good tailor is needed to look at the person, compare it to the best available size and model made, and size it to that individual accordingly. Similarly, the “soft” data used in medical practice are being used to customize the patient’s best treatment plan, diagnosis, and advice.
An 89-year-old grandma comes to the office on Friday afternoon, 3 p.m., with external otitis. She is ambulating with a walker and lives with her husband, who has macular degeneration. The weather forecast is a winter storm for the long weekend, and they do not have anyone in town. The next is the single mom who brings her 8-year-old boy with autism, with external otitis, who is flying the next day to Orlando for their long-awaited dream trip. Otowick is indicated for both.
I will clean the grandma’s ear, place the Otowick, and have them wait in the waiting area for an hour, making sure that they are comfortable and have assistance from staff in case of need. I remove the Otowick after an hour and clean the ear again before they leave with instructions on how to place drops for the next few days and water precautions, and a follow-up call the next day. For the autistic child, Otowick is placed and kept, and I will instruct his mom to put the two or three drops of Ciprodex or similar every two or three hours until their scheduled flight to keep it moist. Remove the Otowick before the flight and continue four drops twice a day with water precaution instructions, including the use of a hair dryer after a shower or any water exposure. And of course, there are other options and acceptable approaches for both cases based on the place of practice and preferences of the provider, for which all could work. But the point is, this type of practice can be easily challenged by EBM while completely accepted and backed by CBM. A certain range of deviation from EBM, therefore, is inevitable but should be acceptable based on the best available soft data and the artistic view and experience of the provider.
EBM is just a framework and should not be abused by policy makers and private payers to justify unfair reimbursement and marginalize practices that do not conform to these standards. EBM is helpful, true, but custom-based medicine should be equally claimed and accepted as an individualized standard of care for our day-to-day practice.
Physicians and healthcare providers are similar to tailors in many ways, trying to customize their practice based on the social, cultural, economic, and geographic situations of the patient.
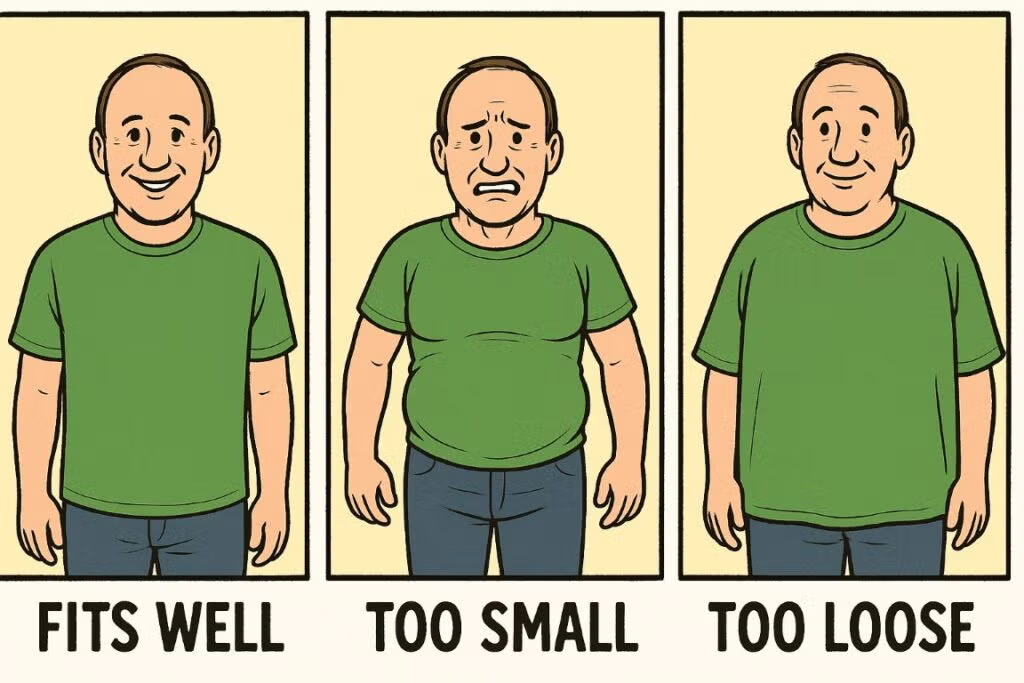 Imagine the look and dress of the people if we insist on dressing everyone only in standard model-based sizes!
Imagine the look and dress of the people if we insist on dressing everyone only in standard model-based sizes!
Dr. Ahmadizadeh is an otolaryngologist and assistant professor in the department of otolaryngology at Northwell Health in New Hyde Park, N.Y.

A powerful reminder that medicine is both science and art. CBM isn’t opposed to EBM…it completes it. Nice article, Dr. Ahmadizadeh.
Very informative and relevant to daily medical practice
Thank you for sharing your wisdom! Excellent advice and insight in today’s “standard of care” practice by new generation of doctors.
Well said!