© Hein Nouwens / Shutterstock
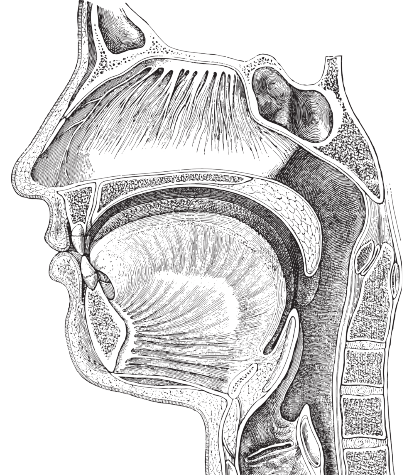
Figure 1. Tk
Introduction
A thyroglossal duct cyst (TGDC) is one of the most common congenital anomalies of the midline neck. Surgical removal is necessary principally due to the possibility of recurrent infection, with postinflammatory cosmetic deformity, aerodigestive tract compromise, and the rare instance of potential malignancy being additional concerns. The most efficacious procedure for avoiding recurrence and ensuring eradication of the disease is the Sistrunk procedure. Dr. Sistrunk never officially published a recurrence rate with his publication in 1920 (Ann Surg. 1920;71:121-122.2), but a recent systematic review and meta-analysis have documented a recurrence rate of 6% to 10.7% with the Sistrunk procedure performed in a classic or modified fashion (Int J Oral Maxillofac Surg. 2015;44:119-126; J Pediatr Surg. 2013;48:222–227). Recurrence is mostly associated with incomplete resection of the central portion of the hyoid bone and perihyoid disease (Laryngoscope. 2010;120:1773-1778). This report expands on the senior author’s prior description of the posterior hyoid space (PHS) as it applies to a modified Sistrunk procedure. The associated video correctly illustrates this anatomic area and provides surgical footage of its application.
Method
All of the research planning, strategies, data collection, and analyses were completed in accordance with the World Medical Association Declaration of Helsinki. After obtaining institutional review board approval, a retrospective chart review was undertaken on modified Sistrunk procedures performed at our institution from January 2017 to November 2020. A total of 100 patients were identified whose procedures were performed by 10 operating surgeons within the division of pediatric otolaryngology. No revision surgeries were included in this study. All patients included had a postoperative diagnosis of TGDC and were under the age of 21 years (range 11 months to 20 years). Their demographic characteristics, perioperative findings, and postoperative complications are summarized in Table I. Preoperative imaging—ultrasound in 92%, computed tomography alone in 7%, and MRI alone in 1% of cases—confirmed a normal-appearing thyroid gland in 100% of patients. Minor complications occurred in 10% of patients, consisting of five seromas, one rash, one surgical site infection, and three hypertrophic scars. There were no major complications.
Recurrence is mostly associated with incomplete resection of the central portion of the hyoid bone and perihyoid disease.
Every patient who was included attended at least his or her first postoperative follow-up visit. Patients and their families were educated on recurrence and were instructed to contact our office with any concern. There was one documented recurrence (1%). None of the 99 patients listed as not having a recurrence in this study had ever contacted our office with any concern for recurrence, had evidence of recurrence in our electronic medical record system or in any outside hospital record obtained via Epic Care Everywhere, or had ever requested their medical records from our office. To further ensure the accurate capture of recurrence rate, any patient with in-office follow-up of less than four months was called over the telephone for a phone interview, with a response rate of 64% (30/47). We chose to reach out to all patients with less than four months’ follow-up, as it has been previously reported that if a recurrence is to occur, it will likely happen within the first four months following the procedure (Laryngoscope. 2010;120:1773-1778; Am J Surg. 1986;152:602-605). The longest follow-up time was recorded as the last known contact with the patient/family, whether an in-office visit or a telephone interview, with an average follow-up time of 11.2 months.
Table I. Results.
| Total Patients | 100 |
|---|---|
| Male | 49 (49%) |
| Female | 51 (51%) |
| Neck mass only at presentation | 89 (89%) |
| Fistula at presentation | 11 (11%) |
| History of/current infection at presentation | 36 (36%) |
| Average age at presentation | 6.2 yr |
| Average age at surgery | 6.8 yr |
| Minor complications | 10 (10%) |
| Major complications | 0 (0%) |
| Recurrence | 1 (1%) |
Results
This report further validates the application of the PHS to the modified Sistrunk procedure, limiting the rate of recurrence without increasing the complication rate in thyroglossal duct surgery.