Sinonasal and skull base tumors pose unique challenges to patients, their families, and the clinicians who care for them. Their rarity limits the availability of clinical expertise, the pace of research, and the strength of public awareness. However, two patient-driven organizations, the Chordoma Foundation and SMARCB1 Hope, demonstrate how committed advocacy can transform the landscape for patients with rare malignancies.
For this article, we carried out in-depth interviews with key figures of both foundations: Shannon Lozinsky, director of patient services for the Chordoma Foundation, and Cassie and Jean-Baptiste Toulouse, the founders of SMARCB1 Hope. We distill these interviews to focus on the role and power of patient advocacy for otolaryngologists.
Origins in Urgent Need and Personal Tragedy
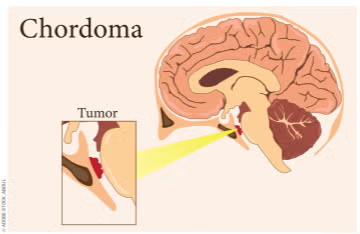
The Chordoma Foundation began in 2007 when Josh Sommer, then a Duke University student, was diagnosed with a skull base chordoma. Finding virtually no patient resources, he and his mother, a physician, connected with a small group of patients online. After his treatment, Josh got a job working with one of the few labs studying the disease, which, fortunately, was based at Duke. This small group of patients and loved ones soon realized the urgent need to unite more patients, researchers, and clinicians into a single, coordinated movement. Starting literally at one family’s kitchen table, the foundation has grown into a global leader in rare tumor advocacy and research.
SMARCB1 Hope was founded by Cassie and Jean-Baptiste Toulouse after the devastating loss of their 23-year-old daughter, Ella, to an aggressive SMARCB1-deficient sinonasal carcinoma in 2020. Lacking established networks, treatment protocols, or community support, they recognized the urgent need to build a resource for patients and families confronting this ultra-rare tumor.
Their mission grew beyond sinonasal carcinoma to encompass all SMARCB1-deficient cancers in order to build a larger, interconnected community and amplify research impact. Recently, they have also partnered with a larger French cancer organization (ARC Foundation) to strategically position SMARCB1 cancers within the broader category of adolescent and young adult cancers, thereby broadening appeal without losing focus on their original cause.
Mission and Core Activities
Chordoma Foundation
• Three Strategic Pillars:
- Research—Establishing and sharing preclinical disease models, conducting in-house research at the Foundation’s dedicated laboratory, driving global collaboration, and supporting chordoma-specific clinical trials.
- Patient Services—Education on the disease, treatment options, and recommendations, navigation to high-volume specialists, and peer support networks.
- Healthcare Improvement— Creation and dissemination of consensus, evidence-based guidelines for diagnosis, primary treatment, and recurrence.
• Patient Navigation Program: Direct access to navigators who provide immediate, personalized guidance, connect patients with experts, and link them to peer communities.
• Community Conferences: Bring patients, caregivers, clinicians, and researchers together, often alongside research workshops, to foster mutual understanding.
• International Outreach: Ambassadors in multiple countries, translated educational materials, and online community platforms ensure global accessibility. SMARCB1 Hope
• Patient Support and Navigation: Provides newly diagnosed patients with clear information, emotional support, and referral to research centers with expertise.
• Research Facilitation: Organized an international symposium in 2023 gathering 30 researchers from multiple SMARCB1 tumor subtypes to explore shared biology (epigenetics, chromatin remodeling) and cross-tumor therapeutic approaches.
• Community Building: Connects patients globally, fosters collaborations between research teams, and promotes awareness campaigns, including patient stories and forthcoming documentaries.
• Strategic Partnerships: Cassie and Jean-Baptiste recently launched the Ella Toulouse Foundation for Adolescent and Young Adult Cancers under the aegis of the ARC Foundation. By broadening their scope and working with this big cancer organization widely known in France, they aim to attract more attention to solid tumors with epigenetic mechanisms and leverage ARC’s scientific review committee and funding power.
The “Secret Sauce” of Effective Advocacy
When asked why their organizations succeeded where others have struggled, leaders from both organizations pointed to deep patient focus as the central factor.
The Chordoma Foundation works to bring together nearly every patient and family affected. The result is a close-knit, highly engaged community where patients feel genuine ownership of the mission—and where many of the largest donors began as service users.
SMARCB1 Hope credits persistence, relationship building with key researchers, and willingness to adapt scope without losing identity. They stress that effective advocacy requires readiness for a decades-long commitment, strategic use of limited funds, and humility to keep the mission above personal ego.
Both groups emphasize that advocacy is not simply “raising awareness,” but is sustained, strategic work to connect the right people, push promising research forward, and ensure that patients are informed and supported from diagnosis onward.
What Otolaryngologists Should Know—and Do
While otolaryngologists may only encounter a handful of these rare tumors in their careers, they play a pivotal role in initiating connections that can change patient trajectories.
Key Takeaways for Clinicians:
- It matters where the patient is treated—For both chordoma and SMARCB1-deficient sinonasal carcinoma, surgical expertise, radiation modality, and multidisciplinary coordination can significantly affect outcomes. Early referral to centers with demonstrated experience is critical.
- Encourage second opinions—Especially for rare cancers, patients often enter a treatment “funnel” that is hard to exit. Urge patients to seek a second opinion, not necessarily to change treatment plans, but to validate them and provide reassurance.
- Identify and connect to disease-specific groups early—Clinicians should be proactive in referring patients to disease-specific organizations. These groups provide immediate access to vetted information, expert lists, peer support, and often research opportunities.
- Recognize the emotional and informational gap—Newly diagnosed patients with rare cancers often find their local care teams cannot fully answer disease-specific questions. A single phone call from a knowledgeable navigator or peer can alleviate fear and confusion.
- Collaborate across institutions— Both organizations note the importance of clinicians reaching out to disease experts, even outside their own institutions, for consultation or co-management.
- Support research through referrals—Whenever possible, encourage tumor tissue donation to relevant research efforts. For ultra-rare diseases, every sample can be invaluable.
Lessons for Generalizing Advocacy Models
Chordoma Foundation emphasizes that even without major research budgets, any rare disease community can replicate certain fundamentals:
- Build a patient database and maintain regular, meaningful contact.
- Provide direct access to a real person for guidance.
- Facilitate peer-to-peer connection to reduce isolation.
- Identify and share specialist lists so patients can find experienced providers.
- Partner with clinicians to ensure guideline dissemination and appropriate referrals.
Similarly, SMARCB1 Hope advises would-be advocates to:
- Commit for the long term— meaningful change may take 10-20 years.
- Avoid funding in isolation—seek to leverage established networks and review processes.
- Stay adaptable—be willing to broaden focus strategically to strengthen sustainability.
- Focus on relationships—with researchers, clinicians, media, and other advocacy groups. The Clinician–Advocate Partnership
The interviews reveal a shared vision: Patient advocacy groups and physicians are most effective when they operate as true partners. Otolaryngologists are often the first to diagnose these rare tumors and can:
- Initiate early contact with advocacy groups;
- Provide educational sessions at patient meetings;
- Participate in or host research workshops; and
- Encourage multidisciplinary and inter-institutional collaboration.
By doing so, clinicians not only improve individual patient experiences but also contribute to a broader ecosystem that accelerates progress in understanding and treating rare sinonasal and skull base tumors.
Conclusion
The Chordoma Foundation and SMARCB1 Hope offer compelling case studies in how determined, patient-centered advocacy can change the trajectory for those facing rare cancers. For physicians, these organizations are not just referral destinations—they are potential collaborators, sources of cutting-edge information, and allies in the mission to ensure every patient receives expert, informed, and compassionate care from the outset.
As Cassie from SMARCB1 Hope reflected, “If we bury ourselves in our very narrow field, we’ll go nowhere. We have to be strategic, broaden the scope, and keep building relationships.” And as Shannon from the Chordoma Foundation affirmed, “We couldn’t do any of it without the patients. Staying connected to them is what makes everything else possible.”
For the otolaryngology community, the message is clear: Engage with advocacy early, respect and harness the knowledge of rare disease patients, and work together across disciplines and borders. In rare cancer care, these partnerships are essential.
Dr. Woods is a consultant otolaryngology–head and neck surgeon at Beaumont Hospital/ RCSI, Ireland, an honorary clinical associate professor at the Royal College of Surgeons in Ireland, and co-chair of the Clinical Care and Patient Advocacy Committee of the AHNS Skull Base Surgery Section.
Dr. Cohen is an attending on the head and neck service and surgical director of the Multidisciplinary Skull Base Tumor Program at Memorial Sloan Kettering Cancer Center, and the medical director for Enterprise Access at MSKCC.
Dr. Walgama is an otolaryngologist practicing at Cedars–Sinai Medical Center. He is dual fellowship trained in both rhinology/skull base and head and neck oncology.



Leave a Reply