INTRODUCTION
Explore This Issue
February 2026Tracheotomy placement is an airway management procedure regularly performed by a variety of physicians, most commonly through a percutaneous route (critical care/general surgery) or open surgical approach (otolaryngology). Bedside percutaneous tracheotomy is appreciated for its convenience, quickness, and safety; however, it is not rare to encounter anatomic irregularities necessitating further imaging, a formal surgical tracheotomy, or alternative procedures.
Herein, we report a case in which formal tracheotomy was planned for long-term ventilator dependence in the setting of bilateral vocal fold paralysis. Moments before incision, a visible pulsation was noted in the lower neck. Further imaging was undertaken, which ultimately revealed a high-riding innominate artery within the surgical trajectory. This anatomical variation necessitated an alternative surgical approach for airway management, ultimately in the form of vocal fold lateralization.
The following report illustrates a cautionary tale that is of particular importance to trainees in understanding alternatives to airway management to avoid unintended major consequences.
CASE REPORT

Figure 1. Vocal fold visualization as seen on bedside laryngoscopy. Arrow shows the maximal glottic opening due to bilateral vocal fold paralysis
A 73-year-old woman with a recent upper respiratory tract infection presented to the emergency department (ED) with three days of progressive dyspnea and stridor. Bedside laryngoscopy revealed bilateral vocal fold paralysis (Fig. 1). The patient decompensated in the ED, requiring subsequent intubation and transfer to the ICU, with tracheotomy placement planned for the next day for airway stabilization. Bedside clinical examination of the neck in the ICU was unremarkable, and the patient was taken to the operating room.
In the OR, following anesthesia, surgical positioning, and sterile prep, a visible pulsation was noted in the lower neck. After a discussion between the surgical team and vascular surgery, a decision was made to abort the procedure, given its non-emergent nature, and to pursue further imaging workup. A neck computed tomography (CT) revealed prominent vasculature within the surgical trajectory (Fig. 2A), with angiography confirming a high-riding innominate artery at the level of the upper tracheal rings (Fig. 2B).
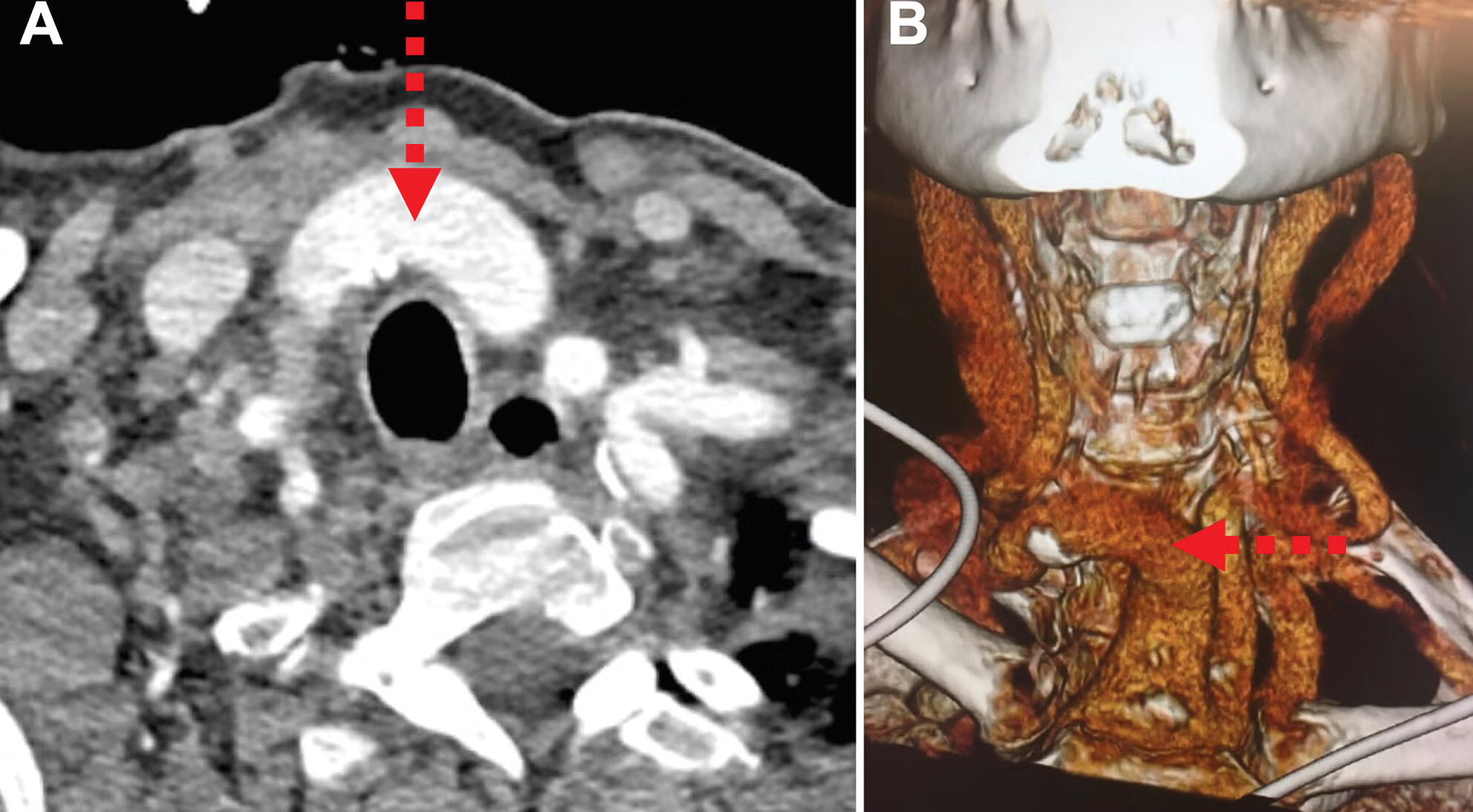
Figure 2. High-riding innominate artery. Axial CT scan of the neck with contrast demonstrating the location of the innominate artery, approximately at the levels of the first and second tracheal rings (A) Three-dimensional vascular reconstruction based on CT angiography. (B) Arrows show the innominate artery obscuring the trajectory for tracheotomy placement.
Vascular, cardiothoracic, and laryngology teams were formally consulted to discuss alternative approaches for airway management for the patient. Ultimately, the decision was made to avoid tracheotomy in favor of bilateral vocal fold suture lateralization performed by the laryngology team. The patient was extubated the following day without subsequent airway difficulty and was able to tolerate food while still having reasonable phonation.
CONCLUSION
Regardless of tracheotomy placement route (percutaneous or surgical), anticipation of anatomic irregularities is essential for patient safety and procedure success. A patient-centered approach that involves discussions with other surgical fields is imperative in determining the best approach for difficult airway securement.
Read the entire article here.
Leave a Reply