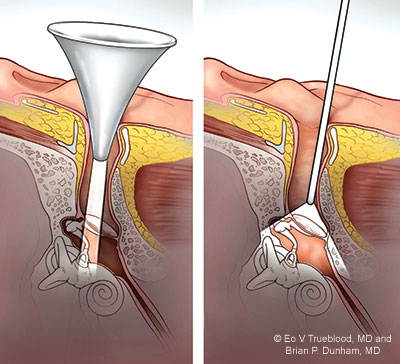
Left: Transcanal microscopic view is limited by the size of the speculum. Right: Transcanal endoscopic view is wider than the microscope.
As strong as the case is for TEES, there are instances when surgeons begin the procedure and then, at some point, have to switch to the microscope after encountering structural anomalies or other unforeseen complications. When that happens, delays in care can result. With this possible complication in mind, a few years back, Daniel Killeen, MD, an assistant professor in the department of otolaryngology–head and neck surgery at UT Southwestern Medical Center in Dallas, decided to explore whether those surgical switches could be more reliably predicted. What he and his colleagues came up with is the antrum-malleus-tegmen (AMT) score, a novel computed tomography (CT) screening tool that can be used to determine pre-operatively whether a patient is a strong candidate for TEES versus the microscope-guided approach.
Explore This Issue
July 2025Dr. Killeen first published on the efficacy of this predictive tool in 2019 (Otol Neurol. doi:10.1097/MAO.0000000000002395), but he’s using those findings to effectively guide current cases and recently described its evolving utility at the AEESSG annual meeting. He began by summarizing the key data. The 2019 study included 59 cholesteatoma patients, 39 of whom were treated with TEES and 19 who required conversion to an open mastoidectomy. After controlling for “a host of confounders,” including patient age, gender, disease laterality, and revision surgery status, Dr. Killeen and his co-investigators identified three independent radiographic predictors for having to convert to an open mastoidectomy. Those risk factors—each of which is given numerical values used in the scoring system—were antrum opacification (P=0.023), malleus erosion (P=0.044), and tegmen erosion (P=0.023) (Figure 1). Looking at the data another way, they found that when two or more of the following conditions were met—an aerated antrum, an intact malleus, and an intact tegmen—TEES was achievable in 88% of cases.
If you’re a good surgeon with a microscope, you’ll always achieve better outcomes than would a bad surgeon with an endoscope. This is not a magic wand we all can wave at a patient with middle ear disease. —Daniel Killeen, MD
But the scoring system’s ability to warn against TEES is often the one that guides Dr. Killeen in his practice. “Just last week I had a cholesteatoma patient who had two of the three red-flag imaging findings we identified in the paper—antrum opacification and malleus erosion—and I saw that as reason to not do the procedure endoscopically,” he said. Interestingly, as he began the surgery guided by the microscope, the extent of disease looked fairly limited, “and I thought, dang it, maybe I could have done this with the endoscope. But sure enough, as I progressed, the cholesteatoma kept extending into the mastoid. So I actually was glad I had used the microscope from the beginning, because it saved me the considerable time that would have been lost converting from endoscopic to open surgery.”
Making the Right Choice
For some ENT surgeons, choosing between an endoscope and a microscope often comes down to skill and experience. “If you’re a good surgeon with a microscope, you’ll always achieve better outcomes than would a bad surgeon with an endoscope,” Dr. Killeen said. “This is not a magic wand we all can wave at a patient with middle ear disease.”
Dr. Killeen also stressed that not all studies comparing TEES versus microscope-guided surgery show clear superiority for the endoscopic route. “At best, we can say it’s non-inferior,” he said, citing, as an example, a study he co-authored showing similar rates of post-operative closure in tympanoplasty patients treated with either route (Otol Neurotol Open. doi:10.1097/ONO.0000000000000016).
He did acknowledge that TEES spares a patient a postauricular incision and the longer recovery that entails. “But I have to say that most patients are not bothered by that [recovery],” Dr. Killeen said. “So if the microscope is what you excel at as a surgeon, stick with it. Now, do I think that learning the endoscope is quite as hard as some surgeons might assume? Probably not. But I also realize that if you have four or five procedures scheduled on a given day, and the endoscope will initially be about an hour slower per procedure for folks new to it, I absolutely get why you might not want to switch.”
Dr. Golub agreed that TEES will never be an attractive option for all ENT surgeons. But he certainly wants the procedure’s adherents to grow. “That’s why my personal goal is to bolster TEES adoption nationwide, by training both younger and older physicians so they can have this valuable tool in their middle ear surgery armamentarium.”
Leave a Reply