Parotidectomy.
© Nilesh Vasan, MD
SAN DIEGO—Head and neck surgery often involves finesse and preference, and techniques developed by a surgeon over time can be valuable to others if they’re shared. In that spirit, a panel of experts offered their insights and tips on a few common surgical procedures at the Annual Meeting of the American Academy of Otolaryngology-Head and Neck Surgery.
“There are tons of unmeasured variation, how we all do things differently,” said panel moderator Alexander Langerman, MD. “Wouldn’t it be cool if we could get a sense of how everybody’s doing everything so we have a bunch of tools in our box?”
The panel offered advice on glossectomy, tonsillectomy and neck dissection, and parotidectomy.
Glossectomy “Geppetto” Technique
Daniel Deschler, MD, vice chair of academic affairs for otolaryngology-head and neck surgery at the Massachusetts Eye and Ear Infirmary in Boston, presented the case of a 52-year-old man with a slow-growing lesion on the right lateral tongue that was 1.9 cm by 1.1 cm by 9 mm.
A biopsy found it was moderately differentiated squamous cell carcinoma. A computed tomography (CT) scan found there was no deep extension to the midline. There was no nodal involvement.
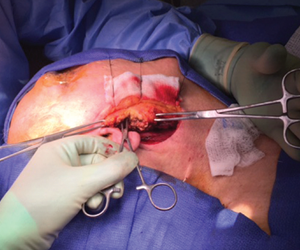
Dr. Deschler performed a partial glossectomy, with selective neck dissection, even though this was an N0 tumor, because the evidence shows there’s a benefit in doing so in these cases (N Engl J Med. 2015;373:521-529). For the Geppetto technique, named after the fictional woodcarver who crafted Pinocchio, Dr. Deschler offered these suggestions:
- Place sutures around the tongue lesion at 1 cm from the edge to get a 1 cm margin.
- Control the edges with the strings, like a puppeteer, as you do the mucosal incisions.
- Consider using a Colorado needle for the Bovie, and a harmonic scalpel. With these, he said, you get little to no bleeding and little char, making the sample easier for the pathologist to evaluate. “There’s not a lot of associated burn.”
- Aim for a specimen shaped “like a canoe”—deeper in the middle and more narrow and more shallow at the ends. This gives a well-defined specimen without taking extra tongue, he said.
- Mark the specimen with string. Dr. Deschler leaves a shorter string on the superior edge of the specimen—both “shorter” and “superior” start with “S”—so there’s no confusion once the specimen is at pathology.
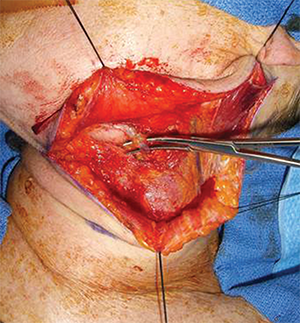
Division of the facial vein followed by superior retraction of the submandibular gland protects the marginal mandibular nerve without the need to identify it, while affording wide exposure to access level II of the neck.
© Courtesy Jeremy Richmon, MD
There were different views on margins in these cases. Panelist Nilesh Vasan, MD, associate professor of otolaryngology-head and neck surgery at Oklahoma Health Sciences Center in Oklahoma City, said he likes to use the sutures as well, but prefers 1.5-cm margins—a study he worked on showed that this size margin resulted in a clear margin in 96% of cases.
In these cases, he acknowledged, sometimes a flap is needed to reconstruct. “We do have wide margins but oftentimes, depending on what the status of the neck is, they may not need any further adjuvant treatment,” he said. “I’ve never really worried about the defect. My job is to get that cancer out with clear margins.”
Dr. Deschler said he would be worried about “bringing in uninvolved tongue at either edge to get it around the back” and that he can often have patients leave with no perineural and no perivascular involvement and clear margins with more minimal morbidity.
TORS for Tonsillectomy and Neck Dissection
Jeremy Richmon, MD, director of head and neck surgery robotic surgery at Massachusetts Eye and Ear Infirmary in Boston, offered these suggestions for transoral robotic surgery for tonsillectomy and neck dissection:
- Never bury the tip. “As soon as the tip of your instrument is buried and you can’t see what it’s cutting into, there are going to be issues with bleeding.”
- Always perform a lot of blunt dissection when you’re looking for vessels.
- Make sure the incision isn’t too low, too high, or too small. “You don’t want to work in tunnels, especially cleaning out Level IIb.”
- Consider avoiding the marginal mandibular nerve. “For true level I neck dissection, it’s not necessary.”
- Dr. Richmon prefers not to use muscle relaxation. “I want to know whether that shoulder is being stimulated during the case.”
- Tension is critical when dissecting over the internal jugular vein. “The two areas of danger are high in the IJ and low, where you’re pulling the IJ over and could end up corkscrewing it, folding it on itself. So you have to identify the IJ high and low so you know where you’re dissecting and make sure you don’t accidentally nick that.”
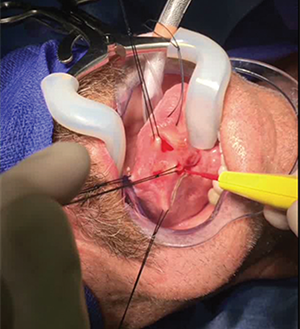
Parotidectomy
“Geppetto” technique for partial glossectomy.
© Courtesy Daniel Deschler, MD
Dr. Vasan offered these suggestions for parotidectomy in the case of a 60-year-old patient with bilateral masses:
- Generally, he suggested a fine needle aspiration for these lesions, but he agreed that if the analysis is done outside your own center and the accuracy rate is low, it could call into question whether the procedure is worth it.
- Preserve the greater auricular nerve, if possible, which it usually is if the lesion is benign and not massive.
- With your incision, don’t go all the way into the neck, but just anterior to the palpable mass. “You don’t have to make a really large incision,” he said.
- Make a lot of headway with the first incision. After that first cut, have your resident or assistant retract the tissue toward you rather than away from you, he said. “If you would just do all of those retractions toward the surgeon, the parotid is back into its normal anatomical shape,” he said. If the seventh cranial nerve is visible, you can divide a lot of tissue right away.
- Consider using a dermal fat graft on reconstruction. “A dermal fat graft actually gets quite long-term beneficial results.”
Dr. Deschler said that, in his experience, it’s possible to get good results without using a dermal fat graft, which is a very involved process.
“Over the last decade, I’ve found that by mobilizing remnant tissues in the area,” either by raising the sternocleidomastoid muscle forward or using the remaining areas of the parotid,“I’m usually able to mask the defect very nicely.”
Thomas R. Collins is a freelance medical writer based in Florida.
Take-Home Points
- Using sutures to demarcate the margin in a partial glossectomy can be a useful technique.
- Consider using blunt dissection when looking for blood vessels.
- Maintaining tension is critical when dissecting over the internal jugular vein.
- After the first parotid incision, retracting the tissue toward (rather than away from) the surgeon can offer better access.