INTRODUCTION
Open surgical treatments for laryngotracheal stenosis in adults commonly include primary resection with anastomosis, such as cricotracheal resection (CTR)/tracheal resection (TR) or staged laryngotracheoplasty (LTP). The indications, techniques, advantages, and disadvantages of these two approaches differ. Airway resection with primary anastomosis is optimal for shorter-segment (<3 cm), high-grade (Grade 3–4) stenosis, and has maximum potential for creating normal luminal diameter. Additional benefits include a single-stage procedure not requiring stent placement; however, a tension-free anastomosis is challenging in long-segment stenosis (>4 cm). High anastomotic tension may lead to anastomotic dehiscence, which is a serious and possibly fatal complication. Other risks include glottic airway edema or vocal fold paralysis due to proximity of anastomosis to the vocal folds or injury to the recurrent laryngeal nerves (RLN), respectively.
LTP is an alternate technique for open airway management when the stenosis is not amenable to primary resection and anastomosis. LTP is preferred in cases of long-segment or multilevel stenosis, infraglottic involvement, or when primary resection is not possible due to excessive anastomotic tension. LTP does not require dissection lateral or posterior to the trachea, thus decreasing the risks of RLN or esophageal injury; however, LTP is a multistage surgery that often necessitates maintaining a stent such as a T-tube between stages. Additional limitations include decreased efficacy in addressing high-grade stenoses, risk for persistent anterior wall collapse, and poor mucociliary clearance.
In this report, we highlight a unique hybrid surgery technique combining the respective benefits of both primary resection with anastomosis and LTP. The hybrid procedure is best suited for the management of complex long-segment or multilevel airway stenosis that is not optimally treated with either procedure alone. In the proposed technique, high-grade subglottic or proximal tracheal stenosis is treated with resection and anastomosis, and the remaining tracheal stenosis, the tracheostoma site, or tracheomalacia is treated with the LTP technique. This leads to better results than using either surgical approach individually and successful long-term decannulation of the tracheostomy-dependent patient.
METHODS
The hybrid procedure commences with airway assessment using suspension direct laryngoscopy and bronchoscopy under general anesthesia. The patient is ventilated via a flexible endotracheal tube through the existing tracheostomy site. The length and severity of stenosis are determined to plan for resection and anastomosis.
The neck is prepared and draped in standard fashion for open-airway surgery. A horizontal cervical incision incorporating the existing tracheostomy is made. Subplatysmal flaps are raised from the thyroid cartilage to the clavicle. Dissection is performed in the midline to divide and lateralize the strap muscles. The thyroid gland is divided in the midline and the laryngotracheal complex is skeletonized from the thyroid cartilage to the sternal notch. Substernal pre-tracheal dissection is performed bluntly with finger dissection, or mediastinoscopy when needed, to mobilize the trachea.
Intraoperative flexible bronchoscopy is performed to identify the superior level for airway resection. Ideally, the airway stenosis is managed by primary resection and anastomosis. The decision to perform a hybrid procedure depends on the surgeon’s comfort and experience with long-segment resection and mobility of the trachea for tension-free anastomosis. If tension-free anastomosis cannot be achieved after tracheal mobilization and other release maneuvers, a hybrid procedure is performed. The high-grade stenosis is resected and anastomosed, and the remaining stenotic tracheal segment is treated with tracheoplasty.
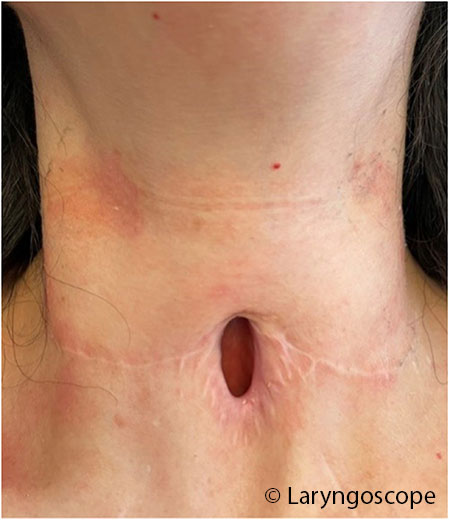
The tracheoplasty is a staged procedure that incorporates the existing tracheostomy site. The involved anterior tracheal stenosis is incised vertically. Then, the superior and inferior skin flaps are advanced and approximated to the tracheal edges using interrupted 3-0 polyglactin (Vicryl) half-mattress sutures. The patient is admitted for post-operative airway management for one week to allow anastomosis maturation. A secondary procedure may be performed to place a T-tube stent spanning the LTP stoma and extending superiorly to the subglottis, which allows for phonation as the airway matures during the healing phase. The anterior wall is reconstructed in multiple layers, over about three to six months, when the stoma has matured (Figs. 1 and 2). Two illustrative cases are presented below.
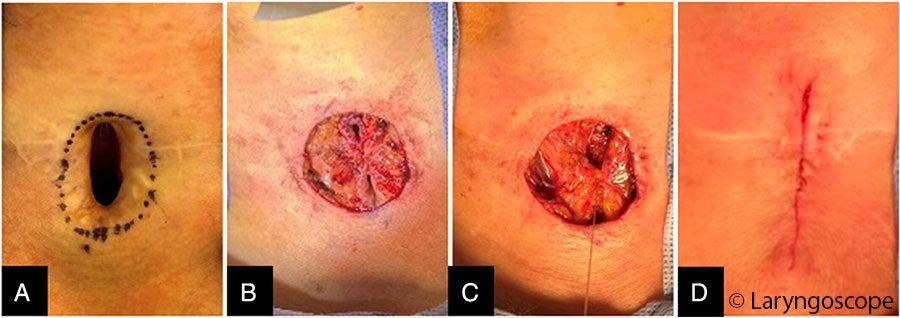
FIGURE 2: Multilayer closure of laryngotracheoplasty stoma after stoma maturation. (A) Stoma is marked with adequate skin width to invert and close the tracheal defect. (B) Skin has been inverted and the initial interrupted Connell suture has been placed. (C) Strap muscle closure has commenced. (D) Final skin closure before application of skin adhesive (Dermabond).
RESULTS
Case 1
A 56-year-old female with a complex medical history, including kidney transplantation, coronary artery disease, type 2 diabetes mellitus, and obesity, was referred for airway management. She had required prolonged intubation followed by tracheostomy due to COVID-19 pneumonia. She was decannulated after three months but required an urgent second tracheostomy several months later due to interval development of airway stenosis. She subsequently failed four endoscopic treatments (CO2 laser resection, balloon dilation, steroid injection, and mitomycin C application). Airway assessment under anesthesia revealed grade 4 subglottic stenosis and a long-segment tracheal stenosis to the tracheostomy site, with a total length of 5.5 cm. The anterior tracheal wall had poor structural integrity due to the two prior tracheotomies. Due to the history of COVID-19, there was significant scarring of the airway to the mediastinum, resulting in poor mobilization of the trachea despite mediastinoscopy and mediastinal release. As the trachea could not be adequately mobilized to allow resection of the entire segment from the subglottis to the tracheostomy site for primary anastomosis, the hybrid procedure was used. A 2.5-cm section of subglottis and trachea was resected primarily and anastomosed, and LTP was performed for the remaining 2-cm segment of stenotic cervical trachea. One week later, a No. 11 T-tube stent (Boston Medical Products, Boston) was placed. The final stage, involving the closure of the LTP stoma, was performed six months later.
Case 2
A 40-year-old female with a 10-year history of shortness of breath presented with acute dyspnea and was diagnosed with critical grade 3 subglottic stenosis. She underwent endoscopic dilation, but a tracheostomy was also performed due to tissue friability and edema. Over the next three years, she underwent five more failed endoscopic airway procedures (CO2 laser excision, balloon dilation, steroid injection, and topical mitomycin C application). She was then referred for open-airway surgery.
Operative endoscopy revealed high subglottic and tracheal grade 3 stenosis spanning 5 cm and involving the tracheostomy stoma. CTR was performed to address 2.5 cm of proximal grade 3 stenosis. The distal 2.5-cm stenosis spanning the length of her tracheostomy site underwent tracheoplasty. A tracheostomy tube was replaced. A T-tube was not placed due to the proximity of the CTR anastomosis to the vocal folds and post-operative edema. The CTR site was patent and healed at three months post-operatively, and LTP stoma closure was performed at six months.