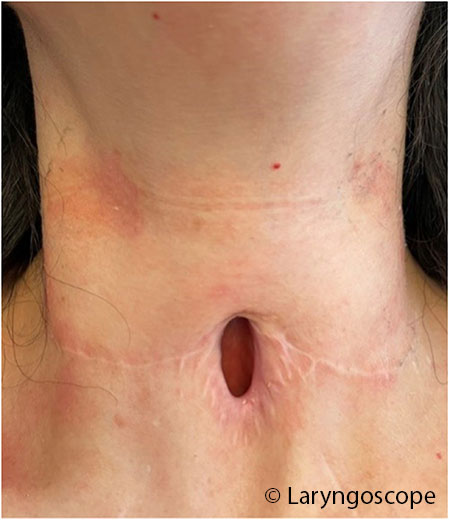
The tracheoplasty is a staged procedure that incorporates the existing tracheostomy site. The involved anterior tracheal stenosis is incised vertically. Then, the superior and inferior skin flaps are advanced and approximated to the tracheal edges using interrupted 3-0 polyglactin (Vicryl) half-mattress sutures. The patient is admitted for post-operative airway management for one week to allow anastomosis maturation. A secondary procedure may be performed to place a T-tube stent spanning the LTP stoma and extending superiorly to the subglottis, which allows for phonation as the airway matures during the healing phase. The anterior wall is reconstructed in multiple layers, over about three to six months, when the stoma has matured (Figs. 1 and 2). Two illustrative cases are presented below.
Explore This Issue
October 2024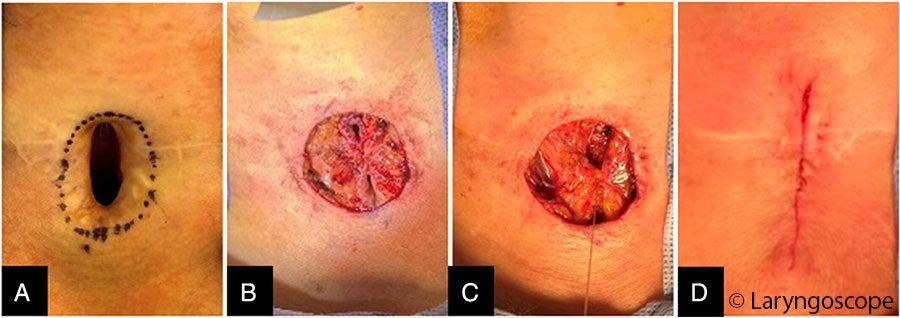
FIGURE 2: Multilayer closure of laryngotracheoplasty stoma after stoma maturation. (A) Stoma is marked with adequate skin width to invert and close the tracheal defect. (B) Skin has been inverted and the initial interrupted Connell suture has been placed. (C) Strap muscle closure has commenced. (D) Final skin closure before application of skin adhesive (Dermabond).
RESULTS
Case 1
A 56-year-old female with a complex medical history, including kidney transplantation, coronary artery disease, type 2 diabetes mellitus, and obesity, was referred for airway management. She had required prolonged intubation followed by tracheostomy due to COVID-19 pneumonia. She was decannulated after three months but required an urgent second tracheostomy several months later due to interval development of airway stenosis. She subsequently failed four endoscopic treatments (CO2 laser resection, balloon dilation, steroid injection, and mitomycin C application). Airway assessment under anesthesia revealed grade 4 subglottic stenosis and a long-segment tracheal stenosis to the tracheostomy site, with a total length of 5.5 cm. The anterior tracheal wall had poor structural integrity due to the two prior tracheotomies. Due to the history of COVID-19, there was significant scarring of the airway to the mediastinum, resulting in poor mobilization of the trachea despite mediastinoscopy and mediastinal release. As the trachea could not be adequately mobilized to allow resection of the entire segment from the subglottis to the tracheostomy site for primary anastomosis, the hybrid procedure was used. A 2.5-cm section of subglottis and trachea was resected primarily and anastomosed, and LTP was performed for the remaining 2-cm segment of stenotic cervical trachea. One week later, a No. 11 T-tube stent (Boston Medical Products, Boston) was placed. The final stage, involving the closure of the LTP stoma, was performed six months later.
Case 2
A 40-year-old female with a 10-year history of shortness of breath presented with acute dyspnea and was diagnosed with critical grade 3 subglottic stenosis. She underwent endoscopic dilation, but a tracheostomy was also performed due to tissue friability and edema. Over the next three years, she underwent five more failed endoscopic airway procedures (CO2 laser excision, balloon dilation, steroid injection, and topical mitomycin C application). She was then referred for open-airway surgery.
Operative endoscopy revealed high subglottic and tracheal grade 3 stenosis spanning 5 cm and involving the tracheostomy stoma. CTR was performed to address 2.5 cm of proximal grade 3 stenosis. The distal 2.5-cm stenosis spanning the length of her tracheostomy site underwent tracheoplasty. A tracheostomy tube was replaced. A T-tube was not placed due to the proximity of the CTR anastomosis to the vocal folds and post-operative edema. The CTR site was patent and healed at three months post-operatively, and LTP stoma closure was performed at six months.