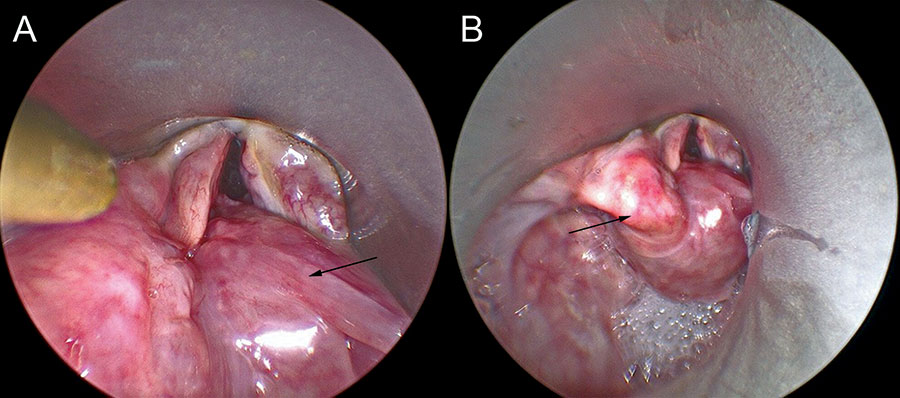
Figure 2: Patient outcomes. Ten days after the original surgery, the patient was taken back to the operating room and the Montgomery laryngeal stent was removed. (A) The right pyriform sinus flap is well healed in the arytenoidectomy defect (arrow). (B) The left arytenoid and its position are preserved (arrow).
E. Laryngeal stenting: The Montgomery laryngeal stent is placed and secured. The anterior cricoid defect is augmented with costal cartilage if necessary. The laryngofissure is closed. The perichondrial flaps, strap muscles, and skin are closed. A Penrose drain is placed. A cuffed tracheotomy tube is then placed and secured. The stent can be removed 10 days after the initial surgery (Fig. 2). Decannulation can occur when the patient is capped without stridor.
RESULTS
From 2006 to 2021, the senior author (PW) performed EL on 11 patients, who all had combined glottic and subglottic stenosis. All the patients had high-grade glottis and infra-glottic stenosis with tracheotomy dependence. All have failed endoscopic interventions. Open surgery using cricoid expansion and/or arytenoidectomy was being considered. The average age of patients who underwent EL was 48.6 years (range 20-69 years). Of the 11 patients, five (45%) had diabetes mellitus, five (45%) had gastroesophageal reflux disease, and two (18%) had both.
Of the 11 patients who underwent EL, eight had undergone prior endoscopic or open procedures. These included endoscopic carbon dioxide laser excision of the scar with dilation and steroid injection, endoscopic partial arytenoidectomy, and thyroarytenoid myectomy with endoscopic transverse cordotomy. One of the patients had undergone prior laryngotracheoplasty. One patient had received a tracheal transplant but then had subsequent glottic and subglottic stenoses, thus preventing decannulation.
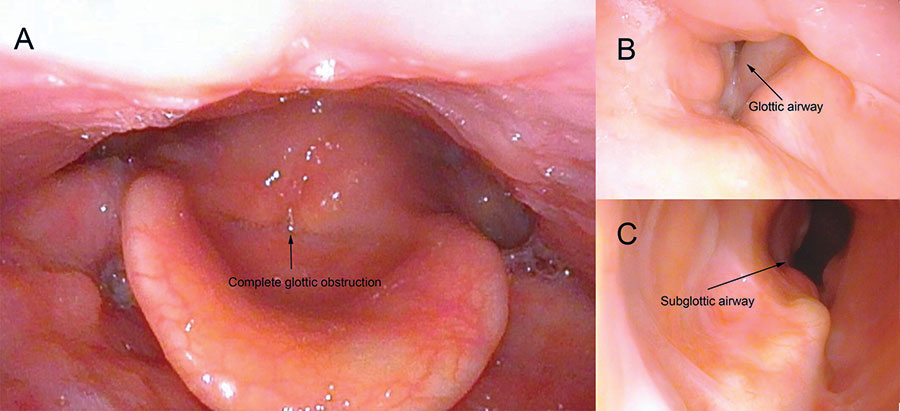
Figure 3: Patient example pre- and post-operatively. (A) Representative photo from in-office flexible fiberoptic laryngoscopy demonstrating complete glottic obstruction with phonation due to posterior glottic stenosis. (B) Representative photo from in-office flexible fiberoptic laryngoscopy one year after expansion laryngoplasty demonstrating a glottic airway of 3 mm posteriorly and (C) showing an open subglottic airway that has been expanded with the costal cartilage.
Of the 11 patients, eight (73%) were decannulated. Figure 3 is a pre- and postsurgical endoscopic view demonstrating complete pre-operative stenosis and the post-operative airway lumen from above and below. The remaining three patients could not be decannulated because of additional tracheal stenosis. The average time to decannulation was 4.6 months post-operatively (range one-13 months). Six patients required additional procedures, including endoscopic dilation and carbon dioxide laser trimming of the pyriform sinus flap after their EL. Only one patient reported post-operative dysphagia. This patient complained of aspiration with liquids 10 years after the initial surgery, which may be due to age-related swallowing dysfunction. She was treated with injection laryngoplasty into the prior arytenoid defect to build up the height of the posterior glottis. All the patients exhibited adequate voice with vibration sources from either the false vocal folds or the pyriform sinus flap.
Leave a Reply