INTRODUCTION
An oroantral fistula (OAF) is a pathological and epithelialized pathway between the oral cavity and maxillary sinus due to extraction of the upper molars, dental infection, trauma, radiation therapy, osteomyelitis, orthognathic surgery, or dental implants. Extraction of upper molars and premolars extraction is considered the most common etiology of OAF (Int J Implant Dent. 2019;5:13; Maxillofac Plastic Reconstr Surg. 2017;39:5; J Nat Sci Biol Med. 2012;3:203–205).
Explore This Issue
December 2022The aim of the OAF management is to repair the defect, restoring the integrity of the sinus and oral cavity and preventing sinus infections. Small fistulas (<5 mm) can heal spontaneously. However, OAF larger than 5 mm or those that have not been resolved within three months usually requires surgical treatment (Int J Implant Dent. 2019;5:13; Maxillofac Plastic Reconstr Surg. 2017;39:5). Choice of the technique for OAF closure depends on multiple factors such as the size, time of diagnosis, infection, height of the alveolar ridge, vestibular depth, further prosthetic treatment, and surgeon’s experience (Int J Implant Dent. 2019;5:). Many techniques have been described for OAF closure, including local and soft tissue flaps, grafts, alloplastic materials, biologics, and metals. However, a rational decision-making process must be followed to choose the most adequate technique (Int J Implant Dent. 2019;5:).
The buccal fat pad flap (BFP) is a simple and reliable flap for the treatment of OAF because of its rich blood supply and location (Maxillofac Plastic Reconstr Surg. 2017;39:5; J Nat Sci Biol Med. 2012;3:203–205). Its overall success rate for OAF closure is around 96.2% (Maxillofac Plastic Reconstr Surg. 2017;39:5). The principal limitation of BFP is the defect’s size because defects measuring more than 4 x 4 x 3 cm have a high risk of dehiscence (Maxillofac Plastic Reconstr Surg. 2017;39:5).
Our group previously described the use of a greater palatine artery (GPA) pedicled flap to repair nasal septal perforations with excellent results and minimal donor site morbidity (Facial Plast Surg Aesthet Med. 2020;22:301–303; Eur Arch Otorhinolaryngol. 2021;278:2115–2121).
This report presents a novel surgical technique for closure of large OAFs based on a combined endoscopic and transoral approach using a GPA pedicled flap and BFP.
METHOD
A 30-year-old man visited our emergency department with a history of four months of purulent nasal discharge and facial pain in the context of upper left molar extraction that did not respond to long-term antibiotic treatment. Nasal endoscopy showed purulent discharge coming from the left middle meatus and a bulging uncinate process. Oral cavity inspection manifested granulation tissue with purulent discharge at the site of tooth 26 (“FDI notation”). Facial and paranasal sinuses computed tomography (CT) was performed, it showed an 11 mm bone defect at the left maxillary floor concerning tooth 26 and a complete opacification of the maxillary sinus with osteomeatal complex obstruction.
We chose a combined endoscopic and transoral approach for OAF closure consisting of a left classical maxillary antrostomy combined with minimally anterior medial maxillectomy using a double-layered flap based on a GPA flap and a BFP.
Nasal cavities were decongested with cotton pledgets soaked with adrenaline 1:10,000 and lidocaine 1%. The nasal septum, nasal floor, and head of left inferior turbinate were infiltrated with a solution of bupivacaine (0.25%) and epinephrine (1:100,000) following a subperichondrial and subperiosteal plane.
First, a left uncinectomy and middle meatal antrostomy were performed. Inflammatory mucosa and purulent discharge were removed using a curved aspirator and forceps. To ensure that no further disease was present, we inspected the maxillary sinus with a 30-degree scope.
A GPA flap was raised in the left nasal cavity. The distance from the anterior nasal spine to the incisive canal was 1.5 cm, measured previously on the patient’s CT, and it was pointed with a surgical marker on the nasal cavity. The posterior vertical incision was performed in the posterior limit of the septum descending across the junction of the soft and hard palate. The superior horizontal incision was performed parallel to the skull base, 1 cm below to preserve the olfactory epithelium.
The anterior vertical incision was performed along with the septal projection of the piriform aperture in an anterior oblique direction, and it was extended downward, 0.5 cm anterior to the GPA exit, to the floor and inferior meatus. Finally, an inferior horizontal incision was performed at the level of the inferior meatus joining both vertical incisions. The flap was elevated and preserved.
Afterward, a minimally left anterior medial maxillary approach was made to ensure an optimal handle of the maxillary sinus and GPA flap. A horizontal incision was made on the lateral nasal wall at the anteroinferior edge of the antrostomy, skirting the head of the inferior turbinate until reaching the piriform aperture. The resultant flap was elevated and displaced posteriorly. The exposed bone was drilled-out at 1–2 mm laterally of the piriform aperture, and then posteriorly in the inferior meatus preserving Hasner’s valve. Bone fragments were removed and a subtotal medial maxillectomy was performed with preservation of the inferior turbinate.
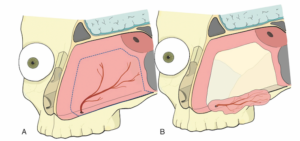
Figure 1. Schematic frontal view of oroantral fistula repair with a double-layered flap: greater palatine artery (GPA) pedicled flap and buccal fat pad flap (BFP). GPA pedicled flap covers left maxillary sinus’s floor and BFP is placed at 26 transorally.
OAF was visualized transorally and the mucosal edges were freshened by removing 1 mm of the margin. From above, a guide point with VICRYL 4/0 was made to the GPA flap close to its anterior edge to facilitate its attachment. The flap was introduced through the subtotal medial maxillectomy, and it was placed to cover the left maxillary sinus floor. Then it was sutured to the lateral mucosal edge of the OAF. A BFP flap was made from a vestibular incision and blunt dissection to reinforce the closure and it was sutured to OAF’s edges with four simple 2/0 silk interrupted sutures (Figure 1).
Finally, the inferior turbinated flap was repositioned and sutured with VICRYL 4/0 to its original position. Silicone nasal splints were fixed to the columella and a nasogastric feeding tube was placed and maintained for five days. No intraoperative or immediate postoperative complications were observed. Complete epithelization was observed at six months post-surgery.
RESULTS
Endonasal–transoral management using double-layered flaps such as GPA pedicled flap and BFP achieve infection resolution, maxillary physiological drainage, and closure of medium and large OAF in a single stage with promising results.