INTRODUCTION
Traditional approaches to laryngotracheal reconstruction have relied on open transcervical approaches. With the growth of endoscopic techniques, there have been multiple advances in minimally invasive procedures to augment airway stenosis in pediatric patients. Among these advances have been the development of endoscopic posterior costal cartilage grafting for posterior glottic/subglottic stenosis (PGS) and bilateral vocal fold immobility (BFVI). This approach has been well described as single and/or double staged procedures in patients with established or electively placed tracheostomy tubes with high rates of successful decannulation and airway patency (Laryngoscope. 2003. doi:10.1097/00005537-200311000-00028; Otolaryngol Neck Surg. 2013. doi:10.1177/0194599812472435; Laryngoscope. 2011. doi:10.1002/lary.21579; Laryngoscope. 2017. doi:10.1002/lary.26200; Laryngoscope. 2021. doi:10.1002/lary.29449). However, the primary risks that exist for the endoscopic technique include the risk of graft dislodgement or migration after extubation. Previous methods have relied on division of the mucosa overlying the cricoid cartilage to access and divide the posterior cricoid cartilage and facilitate placement of the costal cartilage graft.
Explore This Issue
February 2024We describe a novel modification of this approach by preserving the overlying cricoid mucosa and placing the graft in a tight submucosal pocket. We hypothesize that this innovative technique may decrease the risk of graft dislodgement or migration. Additionally, by preserving the overlying mucosa, it may reduce the time to full graft mucosalization, increase vascular supply to the graft, improve secretion clearance postoperatively, and help prevent the need for elective tracheostomy placement.
METHOD
Preoperative Workup
Children with BVFI should undergo an extensive workup to help identify a possible etiology. This can include imaging such as MRI to rule out a Chiari malformation or hydrocephalus. Vocal fold mobility may spontaneously recover up to two years of age. Management is thus dependent on the severity of the presenting symptoms, which can include obstructive sleep apnea, dyspnea, stridor, and dysphagia. Shared decision making between the family and provider is key when deciding on airway interventions or tracheostomy.
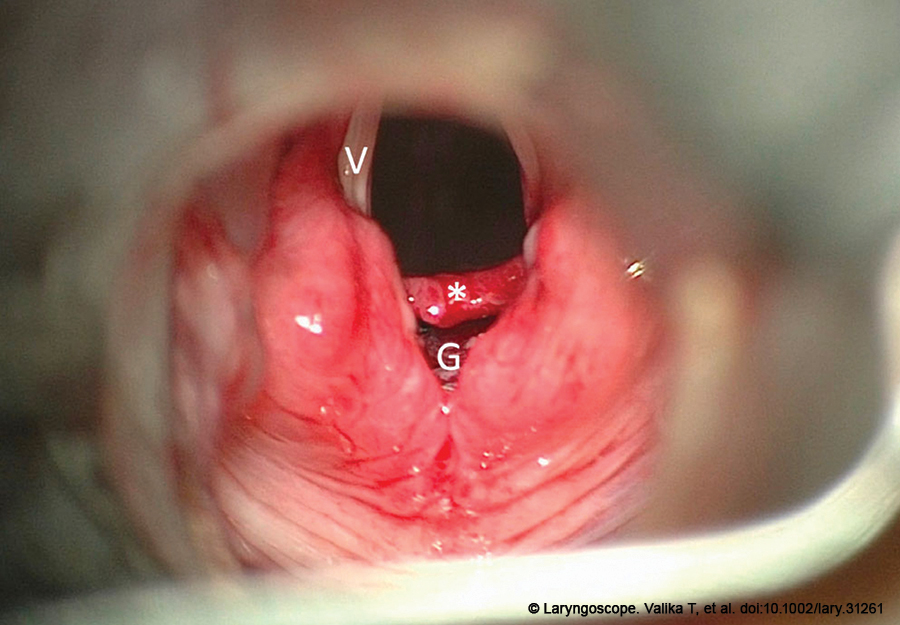
Figure 1. Intraoperative photo after placement of the posterior graft (G). The widely splayed vocal folds (V) are secondary to placement of the graft in between the cricoid cartilage. The mucosal flap (*) remains intact and flush in the airway, with only the proximal aspect of the airway pocket now visible.
When proceeding with any major airway reconstruction surgery, whether for BVFI or PGS, an aerodigestive multidisciplinary evaluation is vital to exclude risk factors such as significant aspiration, reflux disease, or eosinophilic esophagitis. Investigations may include microdirect laryngoscopy, bronchoscopy, bronchoalveolar lavage, impedance probe testing, esophageal biopsies, and instrumental swallowing evaluations.
Surgical Technique
The patient is brought to the operative suite and placed under general anesthesia. Spontaneous ventilation is maintained and anesthesia delivered via insufflation to perform diagnostic microdirect laryngoscopy and bronchoscopy. This ensures the airway is not inflamed, helping optimize the surgical outcome. Preoperative antibiotics (Unasyn, Flagyl if the patient has an allergy) are administered.
The patient is then placed in suspension using an age-appropriate suspension laryngoscope. A vocal cord spreader is placed and suspended to facilitate exposure of the posterior glottis. A straight Sataloff knife is used to make a horizontal incision at the cranial aspect of the cricoid cartilage. Care should be taken not to injure the vocal folds. Using a blunt spatula, a supra-perichondrial mucosal plane is developed and raised from the superior to the inferior extent of the cricoid cartilage.
Raising the flap in this plane provides laxity to the cricoid mucosa, facilitating the expansion surgery goal. If the mucosal flap is raised in the sub-perichondrial plane, the intact overlying perichondrium will prevent the lateral distraction of the cricoid cartilage, negating the surgical goal. In patients with significant scarring of the cricoid mucosa, this technique may not be feasible, as the scar may inhibit lateral expansion and, thus, the traditional method should be utilized.
Preservation of the mucosal flap is vital to this technique. By keeping the mucosa intact, the cilia of the laryngeal lumen are not disrupted, facilitating enhanced clearance of airway secretions in the postoperative period. Once the mucosal flap is sufficiently raised, the cricoid cartilage is divided in the midline using a Sataloff knife, and adequate separation of the cricoid plate is achieved. The airway is sized with uncuffed endotracheal tubes to determine the width of the posterior graft. The patient is then intubated for the harvest and carving of the costal cartilage. Once the carving is complete, the patient is again placed in suspension. The cartilage graft is then gently held with a laparoscopic grasper for insertion. The left flange is secured first and then the right flange is engaged using counterpressure from the spatula. The mucosal flap is then draped down, allowing complete coverage of the graft (Figure 1). Nasotracheal intubation is completed under microscopic visualization to prevent accidental false passage or damage to the mucosal flap.
Postoperative Care
The patient remains intubated in the pediatric intensive care unit for a period of seven to 14 days to optimize graft healing. Anti-reflux medications are initiated and antibiotics are continued for 72 hours until chest drains are removed. Nutrition is delivered via alternative routes. Sedation and ventilator settings are weaned in anticipation of extubation.
On the day of extubation, a single dose of IV dexamethasone (0.5 mg/kg, maximum 20 mg) is given. Microlaryngoscopy is performed to ensure healing of the airway, and the patient is extubated. A videofluoroscopic swallow study, if clinically indicated, is performed once the patient no longer requires supplemental oxygen.
RESULTS
A total of eight patients (age range: 11 months to 10 years old) underwent endoscopic submucosal placement of a posterior graft for either posterior glottic stenosis (n = 6) or bilateral vocal fold immobility (n = 2) between 2021 and 2023 by the senior author. Six patients had a preoperative tracheostomy. All patients were completed in single-staged fashion and had removal of tracheostomy, if applicable, at the same time as the surgical procedure. No patients required elective tracheostomy placement for the procedure.
All patients had a successful outcome, defined by a patent airway and/or tracheal decannulation, if applicable. All grafts showed appropriate mucosalization at the time of the first bronchoscopy. Every patient returned to their preoperative feeding status within six weeks of the procedure. No significant complications (graft dislodgment, airway stenosis) were reported. Additionally, no revision surgery has been required to date.