 Patients with anaplastic thyroid cancer (ATC) who were treated with immunotherapy tended to have better survival in the short term compared to those who were not treated with these therapies, but this benefit didn’t last particularly long, according to findings from a study presented at the Triological Society Combined Sections Meeting.
Patients with anaplastic thyroid cancer (ATC) who were treated with immunotherapy tended to have better survival in the short term compared to those who were not treated with these therapies, but this benefit didn’t last particularly long, according to findings from a study presented at the Triological Society Combined Sections Meeting.
Explore This Issue
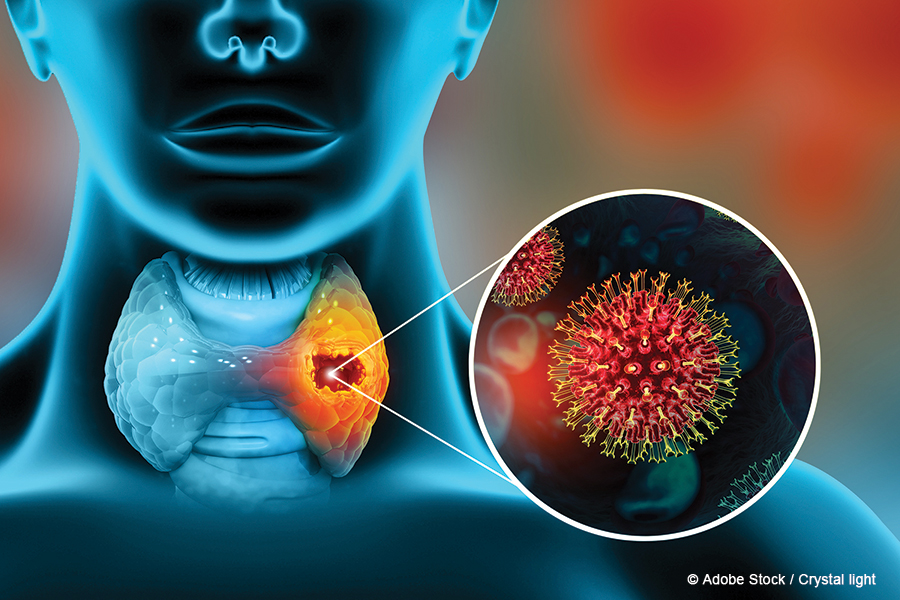
April 2024ATC is a very rare malignancy that’s aggressive and fatal, with a mean survival of just three to six months, said Haidee Chen, BA, the presenter and a third-year medical student at the University of California, Los Angeles (UCLA), who works with Maie St. John, MD, PhD, a professor and chair of head and neck surgery there. Risk factors include being elderly and having previously had differentiated thyroid cancer or radiation exposure, said Chen. These tumors are usually undifferentiated on histopathology and come in spindle cell, squamoid, and pleomorphic giant cell types. Genetic mutations that are typically seen include BRAF, p63 and RAS (Cancers (Basel). 2020. doi:10.3390/cancers12071973).
Targeted immunotherapies have become part of ATC treatment over the last decade or so, boosting recognition of tumor cells and activation of the immune system. But the studies on their effects have been fairly scarce and heterogeneous, Chen said.
The findings come from a retrospective chart review study at UCLA that included 60 patients treated between 2000 and 2023. Researchers pulled data—including demographics, diagnoses and death dates, type of treatment, and mutations—from patient charts in Epic medical software.
Targeted therapy and immunotherapy should be considered strongly when treating patients with ATC. But we have to consider the adverse effects that patients experience, and there should be a discussion of a possible plateau in effects of targeted therapy. — Haidee Chen, BA
The patients were an average of 68 years old at the time of their diagnosis, and 52% were female. BRAF mutations were seen in 32% of cases, p53 mutations in 24% of cases, and p63 mutations in 8% of cases, Chen said. Nearly all of the patients—98%—had had some kind of surgery, and 48% had had a total thyroidectomy, with 44% having had palliative care referrals.
Thirty-eight percent of patients received targeted immunotherapy, and these treatments included dabrafenib, trametinib, pembrolizumab, lenvatinib, sorafenib, encorafenib, and binemetinib. Trametinib, used in 13 cases, and dabrafenib, used in 10 cases, were the most common immunotherapies, explained Chen.
The study authors found that overall survival was significantly better at six months among those treated with immunotherapy compared to those who were not, at a rate of about 80% compared to about 50% (P < 0.05). By 24 months, however, that difference had faded away. “Overall survival improved with targeted immunotherapy,” Chen said. “Over time, unfortunately, this survival was not sustained significantly.”
For dabrafenib and trametinib, patients remained on therapy for five to six months, and the most common reasons for stopping the therapies were fever, neutropenia, and rash.
Researchers also found that nearly 80% of those receiving immunotherapy had a palliative care referral, compared to only about 20% of those not receiving immunotherapy (P < 0.0001). They found no difference between the groups in tracheostomy placement.
“Further studies are needed within ATC regarding novel drugs targeting immune checkpoints, combination targeted immunotherapy, the role of surgical debulking, and palliative care referral patterns and tracheostomy use,” said Chen. Work is also needed on increasing the availability of genetic testing of thyroid malignancies to improve outcomes with precision medicine, and this testing likely needs to be expedited in ATC cases,