INTRODUCTION
Nasal airway obstruction (NAO) is a bothersome condition that negatively impacts a patient’s quality of life and confers a significant economic burden on society. The internal nasal valve (INV) accounts for approximately 50% of nasal air resistance, making it a critical location for symptomology and an opportunity for surgical correction of NAO. The INV can be further divided into the superior and inferior corridors, with these two areas separated by an imaginary horizontal line from the superior aspect of the attachment of the inferior turbinate. Various treatment options have previously been described for addressing the internal nasal valve, including but not limited to septoplasty, turbinate reduction, spreader grafts, batten grafts, flaring sutures, and butterfly grafts.
The butterfly graft (BFG) is a surgical technique for treating nasal obstruction using auricular conchal cartilage to reconstruct the superior corridor portion of the internal nasal valve. In one large study of BFG effectiveness, 444 of 512 patients (86.7%) reported they experienced complete resolution of nasal obstruction; 49 patients (9.6%) reported that their nasal obstruction improved; 19 patients (3.7%) reported no improvement; and no patient reported worsening nasal breathing after BFG placement. Cadaveric computational fluid dynamic models have shown that the BFG provides up to twice as much reduction in nasal airflow resistance compared with the popular spreader graft technique. In recent years, functional and aesthetic outcomes studies have continued to support BFG as one of the most robust techniques to address NAO due to internal nasal valve narrowing.
External contour irregularities remain a significant concern following the butterfly graft procedure. Irregularities are often due to the inherent variability in the thickness of the donor cartilage in the graft, unpredictable bending at the lateral aspects, and difficulty in camouflage in patients with a thin skin soft tissue envelope (SSTE). However, a recently published survey of casual observers visually comparing BFG with the spreader graft group showed no difference in observers’ opinions of the appearance of patients’ noses. Various operative techniques have been described to mitigate the external contour irregularity risk, including decreasing the width and increasing the graft length or scalloping the edges. Despite appropriate counseling and modifications in the primary butterfly graft surgery technique, the senior author observes that a small subgroup of patients is bothered by external contour irregularities after BFG placement surgery.
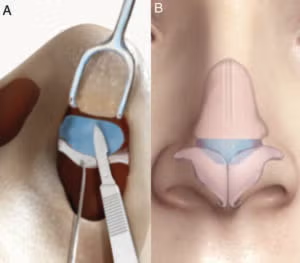
Figure 1. Technique illustration of BFG secondary contouring procedure. (A) Endonasal view of BFG secondary contouring procedure. (B) Schematic view of BFG in position, with red lines showing the most common areas of
contouring.
In this study, we report on the BFG secondary contouring procedure for patients with external nasal complaints following BFG placement and patient-reported outcomes following the procedure. Heretofore, no prior studies discuss this technique and its outcomes. We define BFG secondary contouring as surgical contouring of the BFG at a second procedure following the primary placement surgery (Fig. 1). The aims of our study included describing the surgical technique, presenting demographic factors that may be related or may predispose patients to desiring BFG contouring, and comparing patient-reported outcomes following primary and contouring surgeries. We hypothesized that BFG secondary contouring improves aesthetics while maintaining durable nasal breathing outcomes.
METHODS
IRB approval for this study was obtained from the University of North Carolina Institutional Review Board (IRB 22–2528).
Patient Inclusion
Patients included for review were adults (at least 18 years old) who had undergone primary or revision rhinoplasty with butterfly graft from April 1, 2020, through April 30, 2023. For the case series, we then reviewed patients in this group who elected for BFG secondary contouring.
Data Collection Methods
Demographic information, including age, self-reported sex, and race, primary versus revision initial surgery, and nasal comorbidities, was collected.
The Nasal Obstruction Symptoms Evaluation (NOSE) Score is a five-question validated scale for the evaluation of the problematic nature of patients’ nasal obstruction. The total score (0–100) is taken as the sum of the responses multiplied by five, so the denominator is 100. Higher scores indicate worse nasal obstruction. We used a minimal clinical interval difference (MCID) cutoff of 24 to compare our pre- and post-operative subjective results.
Rhinosinusitis Disability Index (RSDI) is a 30-question validated index for self-reported health-related quality of life (HRQL) related to various rhinologic conditions. The total score (0-120) is the sum of the responses. Higher scores signify worse HRQL due to a nasal condition.
Decision regret scale is a five-question validated scale for patient-reported regret after any healthcare decision. The total score (0–100) is obtained by reverse coding items 2 and 4 (inverse questions), subtracting one from each item, multiplying by 25, and then averaging the subscores. Higher scores represent more regret related to a decision. Prior studies in head and neck surgery have suggested a total decision regret scale (DRS) threshold ≥25 to indicate moderate–strong decision regret.
Clinical Method
During the initial evaluation, demographic information is collected for all patients. Various surgical options for the internal nasal valve are discussed with patients, and the risk of external contour deformities following the butterfly graft is also specifically discussed. NOSE scores and RSDI are obtained at intake for the initial patient visit. After primary BFG surgery, NOSE scores and RSDI are obtained at the post-op month three visit. Patients are asked about external nasal concerns and are offered secondary contouring if there are any concerns. Survey results were not collected beyond three months because this was a small cohort, and one-year data were only available for four out of 10 patients. To allow for adequate resolution of post-operative edema, BFG secondary contouring is typically offered one year after BFG surgery. After secondary contouring of BFG, NOSE scores and DRS are obtained at or after post-op month three. Standard photographs were obtained from the patient during the initial visit, post-operative month three, post-operative month 12, following any initial nasal surgery, and at or after post-operative month three after secondary contouring (Fig. 2).
Operative Method
All patients were operated on by the senior author or under the direct supervision of the senior author. BFG placement is typically performed under general anesthesia along with concomitant nasal procedures, most commonly including revision septoplasty and turbinoplasty. BFG is harvested from conchal cartilage due to favorable elasticity and perichondrium to hold the sutures long term. The graft is placed through an endonasal approach. BFG secondary contouring is offered as an in-clinic procedure or under general anesthesia, but general anesthesia is preferred. The contouring is approached through unilateral or bilateral intercartilaginous incisions; care is taken to place the retractor in the sub-SMAS [superficial musculoaponeurotic system] plane while leaving the BFG “down” to avoid interrupting the adherence between the concave surface of the BFG and the upper lateral cartilages. A fresh 15-blade is then used to contour irregular or bulging aspects of the BFG. Limited local anesthesia is used directly over the site of external contour irregularities. Nasal packing or splints were not used during any surgeries. The current technique involves placement of through-and-through sutures over a small Telfa to close the dead space after contouring.
Statistical Analysis
The Wilcoxon rank-sum test was used to compare pre-operative and post-operative NOSE scores. All statistical analyses were conducted using SPSS statistical software (IBM Corporation, Armonk, NY; Version 28.0.1.1).
RESULTS
Demographics
Three hundred and seventy-four patients underwent BFG initial placement between April 1, 2020, and April 30, 2023. Of this group, 10 patients elected secondary contouring and were the focus of this study. Female patients were the majority (90%), with a mean age of 44.4 years. All patients elected for BFG secondary contouring were white (100%). Concomitant allergies were present in 10 patients (100%) and chronic rhinosinusitis in 9 (90%). One patient reported that a nasal trauma after her initial surgery caused the contour deformity. No infections or extrusions of graft were present in our study group.
NOSE Score
NOSE scores were obtained at the initial visit, three months after the BFG initial surgery, and three months after the secondary contouring. NOSE scores in these timeframes were obtained for all patients (100%). The mean total NOSE score pre-operatively was 61.1 (standard deviation 14.95). Mean total NOSE score after initial placement was 9.4 (SD 14.01), resulting in a net change of 51.7. After secondary contouring, the mean total NOSE score was 13.9 (SD 18.84), resulting in a net change of 47.2 from pre-op and a net change of −4.5 from BFG initial placement.
RSDI
RSDI was obtained during the initial patient visit. A pre-operative RSDI score was obtained for all patients (100%). The mean RSDI pre-operatively was 22, ranging from 3 to 80. RSDI was plotted near decision regret for comparison.
DRS
DRS was obtained at or after three months post-BFG secondary contouring procedure. DRS scores were available for eight patients (80%). One patient whose DRS score is unavailable did not complete the DRS survey during clinic visits and was unable to be reached by phone call or email afterwards. The mean DRS score was 18.75, ranging from 0 to 80. DRS was plotted near RSDI for comparison.
CONCLUSION
BFG secondary contouring is an option for BFG recipients who experience external nasal contour complaints, with the majority who undergo the procedure reporting durable improvements in nasal breathing and nasal appearance. We intend to continue to collect data on BFG secondary contouring to determine if our results and conclusions remain stable in a larger sample size.

Leave a Reply