One of the best tools to use in achieving this higher level of documentation is the relevant International Classification of Diseases, Tenth Revision (ICD-10), listing chronic co-morbid conditions “that may affect a patient’s otolaryngology journey within given care path-ways to accurately predict TCOC,” he added. “If your patient has hypertension or diabetes, or if they are on an anticoagulant or have had a prior cardiac event or any other condition that would affect the morbidity and mortality risk of the condition you are treating within an episode of care, you need to record those conditions as an ICD-10 entry in the assessment section of your SOAP [subjective, objective, assessment, and plan] notes.”
Explore This Issue
November 2024Dr. Harrill stressed that this approach to clinical documentation gives payers what they need to accurately measure value. “Remember, no payer is looking at the uncoded past medical history section of your note, because that is not structured data for machine reading,” he said. “You have to start recognizing now where to put that information in your EHR so that it has transparency to the system. Also, this is not ‘code stacking,’ because only relevant diagnoses matter, such as defined hierarchical care codes [HCCs].” (For more on code stacking, see sidebar.)
He added that “the carrot was laid out for specialists” to bolster patient condition and risk transparency reporting within their medical records and claims billing when CMS updated its evaluation and management (E&M) clinical decision-making standards in 2023. “This shifting emphasis to assessment and plan coding guidelines for FFS parallels the claims-based assessment being built out for episodes of care in VBC,” he said.
Dr. Harrill stressed that “RAF coding is one of the biggest problems now for otolaryngology. We’re where primary care was 12 years ago when it comes to under-reporting patient risk and projected cost of care,” he said. “The good news is we have time because our specialty is on the back end of the VBC integration curve. We can use this time wisely to adopt VBC best practices,”
he stressed.
“Equally important is the defining of outcomes and quality for our specialty and translating that into standards that will be captured and translated
to payers.”
Four Payment Pillars
Becoming VBC ready also hinges on knowing which value-based payment model most affects otolaryngology, Dr. Harrill noted. For that answer, he suggested looking at a framework developed by the Healthcare Payment Learning and Action Network, a group of public and private healthcare leaders that is working to increase APM adoption. The framework (Fig 1)divides APMs into four main categories: traditional fee-for-service, fee-for-service that is linked to some quality and value metrics, alternative payment models that include shared savings with varying levels of risk among stakeholders, and population-based payments (Figure 1). There is a veritable alphabet soup of VBC and APM models within that framework, but for otolaryngology, “know that we are firmly in category 2,” he said.
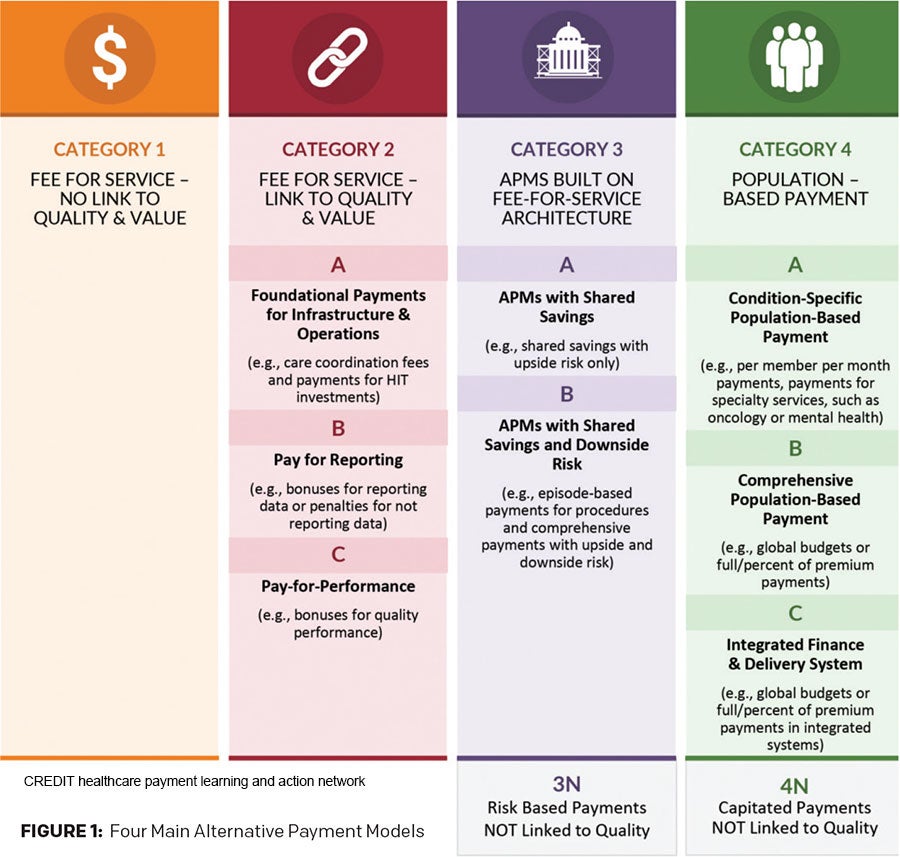 The reasons why are varied, but it essentially comes down to the fact that “our potential savings per patient episode is not that great to be able to share in upside and downside risk,” based on the TCOC for a typical otolaryngologic condition. With other specialties, he noted, one acute hospitalization can cost hundreds of thousands of dollars, and there are multiple ways to impact spend variability for those individual episodes of care. With otolaryngology, in contrast, “our overall spend for chronic sinusitis, for example, is pretty big. It’s just a shallow spend per patient, albeit a very large collective spend for the population. So we still need to find value within that bandwidth.”
The reasons why are varied, but it essentially comes down to the fact that “our potential savings per patient episode is not that great to be able to share in upside and downside risk,” based on the TCOC for a typical otolaryngologic condition. With other specialties, he noted, one acute hospitalization can cost hundreds of thousands of dollars, and there are multiple ways to impact spend variability for those individual episodes of care. With otolaryngology, in contrast, “our overall spend for chronic sinusitis, for example, is pretty big. It’s just a shallow spend per patient, albeit a very large collective spend for the population. So we still need to find value within that bandwidth.”
Head and neck cancer episodes in otolaryngology are a definite exception. Typical head and neck cancer cases, Dr. Harrill explained, involve enough spend variability to “slide nicely” into category 3 bundle payments with the right predictive analytics. “But again, you can’t engage these models unless you understand claims-based analysis and patient RAF scoring,” he stressed. “And that first step is to be able to perform well in the category 2 model care coordination and first-generation quality reporting payment models. For that, you have to have the data documentation and analytics infrastructure in place to tell the patient’s acuity story through ICD-10 coding.”
This urgency is justified, he noted, because “the wheels are already in motion. Whether we like it or not, the market is beginning to build out VBC scorecards to judge us based on our cost variability for a given diagnosis or procedure we’ve recorded in our EHR and claims systems.
Bringing focus to preventing burnout during the transition period will be critical in the intelligent design of VBC programs.” — George A. Scangas, MD