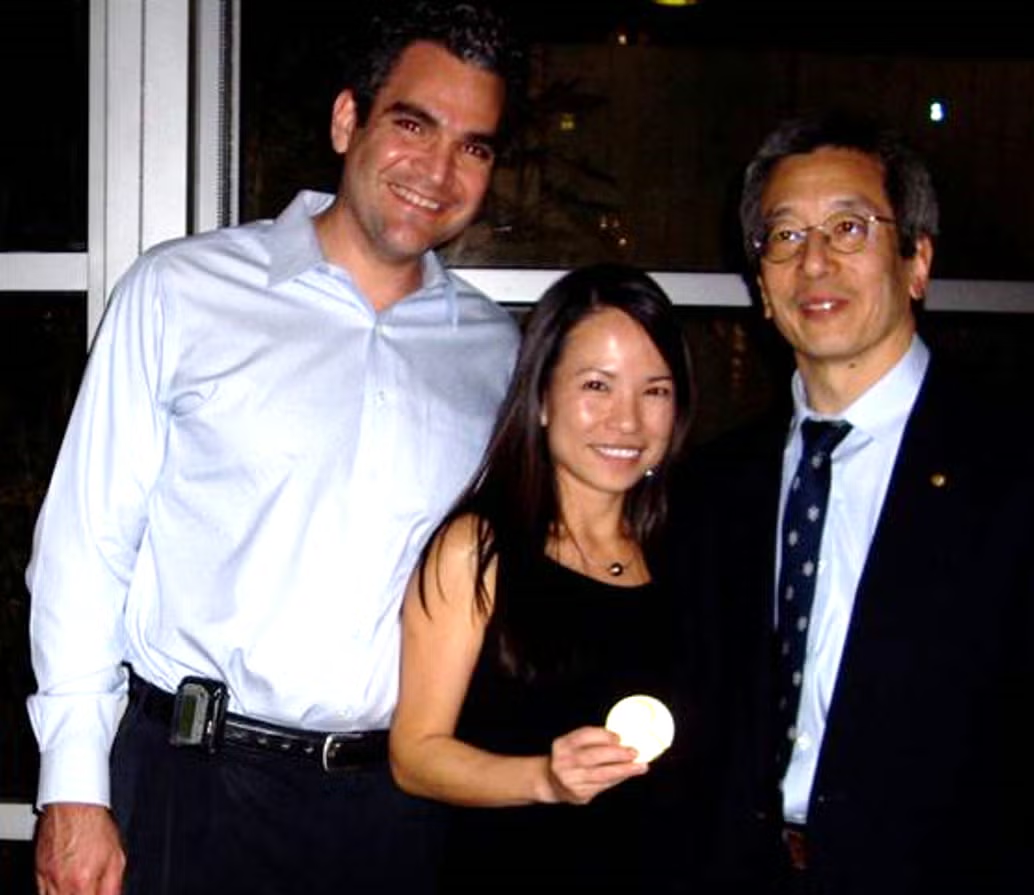
Dr. Lindsay reflects on the Combined Sections Meeting of the Triological Society, highlighting its evolution into a unified, mentorship-focused event that fosters networking, diversity, and research support across all career stages in otolaryngology.