INTRODUCTION
Hypoglossal nerve stimulator (HNS) implantation represents a relatively novel treatment for carefully selected patients with moderate to severe obstructive sleep apnea (OSA) from tongue base obstruction, where the patient is intolerant of continuous positive airway pressure. The technique of implantation has been well described since its introduction to the market in 2014.
Explore This Issue
August 2024Beginning in 2015, HNS began with carefully chosen children with Down syndrome. The first group of children underwent placement of the sensor lead through a separate third incision below the nipple. This approach was modified to a two-incision technique in 2017. In 2023, HNS implantation was approved by the U.S. Food and Drug Administration (FDA) for select patients with Down syndrome (DS). The current recommendations for positioning and placement of the shortened sensor lead are based on adult surgical implant techniques. This technique may be difficult in young children with thin muscular planes or in children with obesity and DS, where the planes between muscles or between muscles and adipose tissue may be difficult to appreciate.
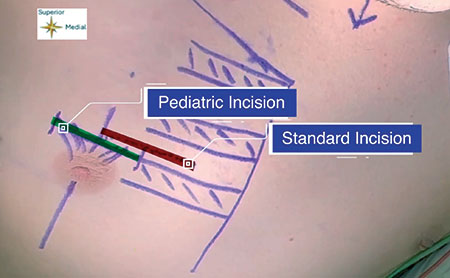
Figure 1: Incision planning. The incision used in this modified technique (green) uses the superior rib margin and the mid-nipple line to base the incision. This is in contrast to previously described standard techniques (red), which base the incision on a distance of 3 cm from the sternum and between two ribs.
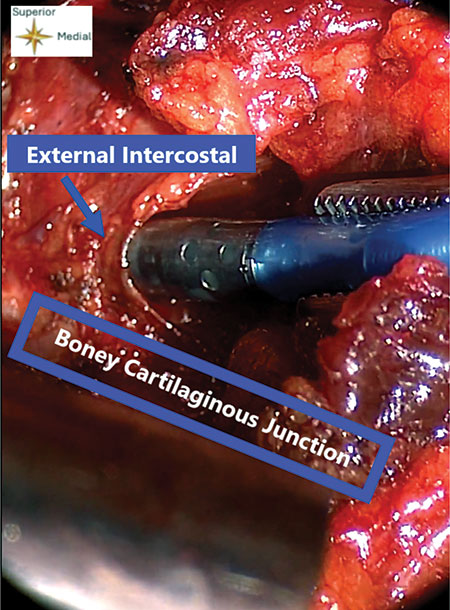
This article describes the technique of the senior author to apply lessons learned from pediatric airway reconstruction and costal cartilage grafting (where the boney cartilaginous junction of the rib is routinely identified), coupled with the anatomic knowledge that the junction between the internal and external intercostal muscles, where the sensor lead will be inserted, lie just on the superior aspect of the rib at the boney/cartilaginous junction. These lessons learned from previous pediatric airway techniques and knowledge of the anatomy allow for a revised technique that may be more time efficient, more straightforward to learn and teach, and safer, with potential for improved patient outcomes.
METHODS
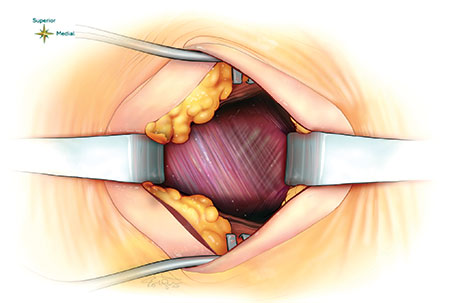
Figure 2: Previously described method of finding the demarcation zone of the internal and external intercostal muscles halfway between the ribs and making a pocket through the external to place the sensing lead between the external and internal muscles.
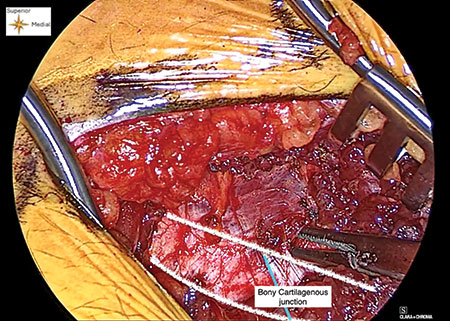
Figure 3: Creating a window. A window or pocket is created with a blunt dissector, and the superior rib surface can be palpated while creating this dissection plane between the external and internal intercostal muscles.
Leave a Reply