It’s no surprise that head mirrors are second only to the stethoscope as one of the most recognizable symbols used in artists’ renderings and Hollywood depictions of a physician. Or that, in most cases, head mirrors are incorrectly shown situated squarely in the middle of the “doctor’s” forehead, much like a shiny, silver bull’s eye instead of flipped down over one eye.
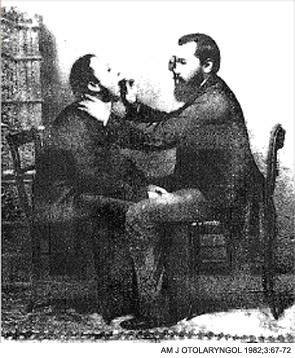
What may be surprising is that this iconic, international symbol of physicians has humble mid-eighteenth century origins, dating back to a French accoucheur named Levert who was fascinated with the intricacies of the larynx. And although doctor’s offices have received more than a few technological facelifts since Levert first dabbled with mirrors in 1743, today’s head mirror has withstood the test of time, resembling the one invented one hundred years later, in the mid 1800s.
Despite demonstrating staying power that weathered the industrial revolution and decades of medical advancements, however, some otolaryngologists question if the head mirror can continue to sustain its relevance and trump its younger technological sibling, the fiber optic headlight.
“I think we’ll see less and less of the head mirror,” said Ron Karni, MD, assistant professor in the department of otorhinolaryngology at the University of Texas Medical School at Houston. “If a physician is more comfortable with the mirror, then he or she should continue to use it. However, battery-powered headlights provide excellent illumination, are relatively cheap and can be transported into the hospital or from room to room in the office.”
D.J. Verret, MD, assistant clinical professor at the University of Texas Southwestern Medical School, recalled using head mirrors in exams during his residency years. Most of the residents he trained with still use the head mirror today, he said. “The head mirror is an excellent method for illuminating the nasal and oral cavity and mirror for indirect laryngeal examination,” he added.
 “If a physician is more comfortable with the mirror, then he or she should continue to use it.”
“If a physician is more comfortable with the mirror, then he or she should continue to use it.”—Ron Karni, MD
Split Decision
One of the reasons headlights gained momentum initially is they require less finesse to adjust where the light is focused, virtually eliminating the need for hours of practice learning to position the head mirror correctly.
“Headlights are easier to use because they don’t require the training and experience that head mirrors do,” Dr. Karni said.
Dr. Karni extolled the virtues of the built-in light source and its power to free otolaryngologists from their offices or a patient from the seated position. “It’s convenient that they don’t require a separate light source,” he said.
Elizabeth A Blair, MD, associate professor of otolaryngology -head and neck surgery at the University of Chicago, likes the portability of headlights. “It’s challenging to use a head mirror on small children who can’t sit still,” she said.
The headlight’s price tag also beckons doctors. When they first went to market, headlights cost thousands, compared to head mirrors, which are priced at around $100. “Now, their price has come down so they’re much more affordable,” Dr. Blair said.
A Constant for Residents
But, despite the headlight’s reduced cost and noted convenience, some residency programs refuse to retire their head mirrors and switch strictly to headlights. Two reasons many teaching programs, like those at the University of California, Irvine and the University of Kansas Medical Center, still require residents to train on head mirrors are that they’re lightweight and cast a very bright and clear light. “The hole in the middle allows for binocular vision,” Dr. Verret said.
Head mirrors are easily transported, too. “I also like that I can take it off easily to tuck in my pocket,” Dr. Blair said. “I prefer to use a head mirror whenever possible because I get a very bright beam of light where I need it, improving my ability to see,” he added.
Another added benefit: You don’t need to worry about your batteries running low or remember to recharge the battery pack.
Then there’s the impact the apparatuses have on your appearance and well being. “Head mirrors are gentler to your head. They’re lighter and less bulky so there’s less chance it will give you a headache after wearing one for several hours or all day. The head band doesn’t get caught in your hair and cause breakage, either,” Dr. Blair said.
Pediatric otolaryngology departments, however, feel differently. “We don’t train residents on the head mirror and we don’t use them in pediatrics,” said Deidre Larrier, MD, resident director of otolaryngology at Texas Children’s Hospital. “Head lights are much easier to use.”
The Head Mirror’s Future
Dr. Blair is quick to note that the specialty shouldn’t automatically discard the head mirror, or move completely to the headlight. “When medicine is looking at ways to be more efficient and cost effective, discarding proven technology for something that is more expensive is questionable,” Dr. Blair said.
Of course, there are always situations in which a headlight is necessary: in the operating room, at the bedside or in the emergency department when a patient is lying down and there’s no light behind the patient allowing use of a mirror.
Many doctors, however, say their colleagues should be familiar with and competent in using both head mirrors and lights. “The practice environment will often dictate which of the two is best suited,” Dr. Blair said.

Leave a Reply