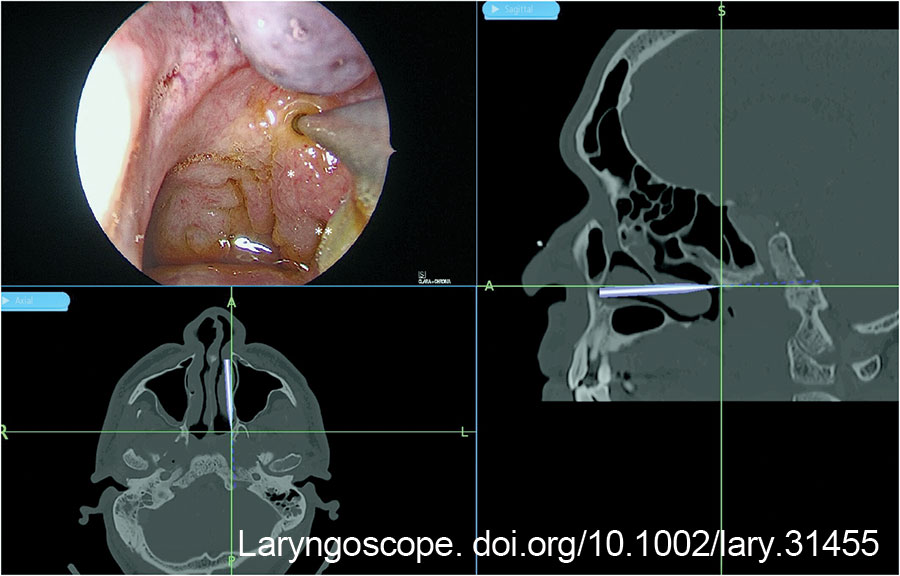
The post-nasal space was examined with a 0-degree Hopkins rod, and the site of the abscess was checked against the image guidance system (Fig. 1). A superficial mucosa biopsy was first performed to exclude nasopharyngeal carcinoma. The biopsy site also served as a marker for the planned incision. A Megadyne 0016 M 6-inch insulated needle point electrode (Ethicon Inc, Cincinnati, Ohio) was used to create a vertical incision medial to the fossa of Rosenmüller, from the roof of the nasopharynx to the level of the Eustachian tube. A vertical incision was preferred over a horizontal incision to avoid lateral dissection toward the Eustachian tube and carotid artery. The salpingopharyngeus muscle served as the lateral landmark to avoid injuring the Eustachian tube orifice (Figure 1).
Explore This Issue
January 2025Hemostasis of surface mucosal bleeding was achieved with adrenaline-soaked patties and suction diathermy to ensure good visualization before deeper dissection. Dissection was deepened with a combination of electrocautery dissection and blunt dissection with a Freer elevator, 8 mm suction, and Blakesley forceps. Constant awareness of the depth of dissection was important to prevent inadvertent injury to the carotid artery. This was achieved by measuring the tip length of the instruments as a gauge of depth, and frequent checks against the image guidance system.
At a depth of 1.3 cm from the mucosal surface, minimal amounts of turbid fluid were encountered posterior–laterally. Blunt dissection was continued toward the source of the turbid fluid till a pocket with necrotic tissue (Fig. 2) was encountered. The necrotic tissue was removed and sent for histological examination and bacteria cultures. The wound was packed with NasoPore (Stryker, Portage, Mich.), which was removed in clinic one week later. The patient was instructed for regular nasal douche.
Aerobic cultures taken from necrotic tissue grew Pseudomonas aeruginosa. Fungal cultures, tuberculosis cultures, and acid-fast bacilli smears were negative. Histology from the superficial biopsy showed mucosa with lymphoid infiltrates with no granuloma or malignancy. Histology of the deep necrotic tissue showed necrotic collagen with neutrophilic aggregates and encrusted bacteria on the surface, with no mucosa or epithelial cells seen. Fluid cultures from the tympanocentesis grew scant Staphylococcus aureus, which was suspected to be contamination from external auditory canal skin flora.
Post-operatively, the patient was kept inpatient for a week of intravenous antibiotic treatment with meropenem, followed by six weeks of oral ciprofloxacin and co-trimoxazole based on antimicrobial culture sensitivities.
CONCLUSION
This study showcases a safe technique for transnasal endoscopic drainage of upper parapharyngeal abscesses. Pre-operative imaging and planning are important to appreciate the relationship to the carotid artery, while intra-operative image guidance and measurement allow the surgeon to maintain anatomical orientation. Taken together, this technique offers effective and safe access for upper parapharyngeal abscess drainage with minimal morbidity and good cosmesis.