INTRODUCTION
The parapharyngeal space is an inverted cone-shaped potential space extending from the skull base to the greater cornu of the hyoid. Early and small abscesses may resolve with antibiotic treatment; however, surgical drainage of the abscess is often necessary for definitive treatment and to obtain tissue for microbiological and histological testing. Parapharyngeal abscesses are usually drained from an external transcervical approach or an intra-oral approach. For abscesses that are centered around the skull base and superior to the level of the soft palate, a transnasal endoscopic route is a feasible approach. Caution needs to be taken to avoid critical structures such as the Eustachian tube and carotid arteries, however.
Explore This Issue
January 2025METHODS
Informed consent was obtained from the patient. Videos and images were de-identified. Institutional review board review was not required based on institutional policy.
A 41-year-old Indian male with poorly controlled diabetes mellitus presented to our hospital with severe right-sided headaches. He had no subjective ear complaints. Examination showed fullness in the right fossa of Rosenmüller, right vocal fold palsy, and right tympanic membrane perforation with granulation tissue and otorrhea. Magnetic resonance imaging (MRI) of the neck and skull base confirmed the diagnosis of right malignant otitis externa with right-sided central skull base osteomyelitis. Mucosal biopsies from the right fossa of Rosenmüller revealed benign histology and tissue culture that grew Staphylococcus aureus. Swab cultures from the right ear grew Candida orthopsilosis and Candida parapsilosis. The patient was treated with a one-week course of intravenous ceftazidime, followed by a five-week course of oral moxifloxacin and six weeks of oral fluconazole concurrently, based on infectious disease specialist recommendations. His headache resolved with treatment, and repeat otoscopy showed resolution of the otorrhea and spontaneous closure of the tympanic membrane perforation. His diabetes was controlled medically, with the improvement of his glycosylated hemoglobin from 11.2% to 7.5% six months later.
An interval MRI scan done six months later showed radiological progression of his skull base osteomyelitis to the left, with a new 2.1 × 1.2 cm rim-enhancing abscess in the left nasopharynx and intracranial spread from the clivus to the cerebellomedually cistern on the right. Computed tomography (CT) scans of the posterior nasal space with IV contrast were obtained for surgical planning and image guidance. Unlike the MRI images, the abscess cavity was not well defined on CT and did not have the typical hypodense rim-enhancing appearance expected of an abscess. He had no symptoms or increase in inflammatory markers despite radiological progression. Nasoendoscopy was unremarkable, with no visible nasopharyngeal bulge or purulence. Otoscopy was normal on the left but showed a clear effusion on the right. Infectious disease physicians and neurosurgeons were consulted, and an urgent culture-directed antimicrobial treatment was advised, to arrest the intracranial spread. The patient underwent transnasal endoscopic drainage of the left nasopharyngeal abscess and right tympanocentesis.
TECHNIQUE
Radiographic measurements from the axial cuts were taken between the depth from the mucosal surface to the anterior abscess cavity wall (9 mm), the posterior–lateral wall (31 mm), and the internal carotid artery (33 mm). On coronal sections, the relationship between the abscess cavity to the sphenoid sinus floor and medial pterygoid plates was noted.
The surgery was conducted under general anesthesia. Image guidance with the StealthStation S7 (Medtronic, Minneapolis, Minn.) system was used. The post-nasal space was washed with half-strength iodine followed by normal saline to minimize contamination with commensal flora. Septoplasty, posterior septectomy, or inferior turbinectomy can be considered to improve endoscopic and instrument access but was not necessary in this case.
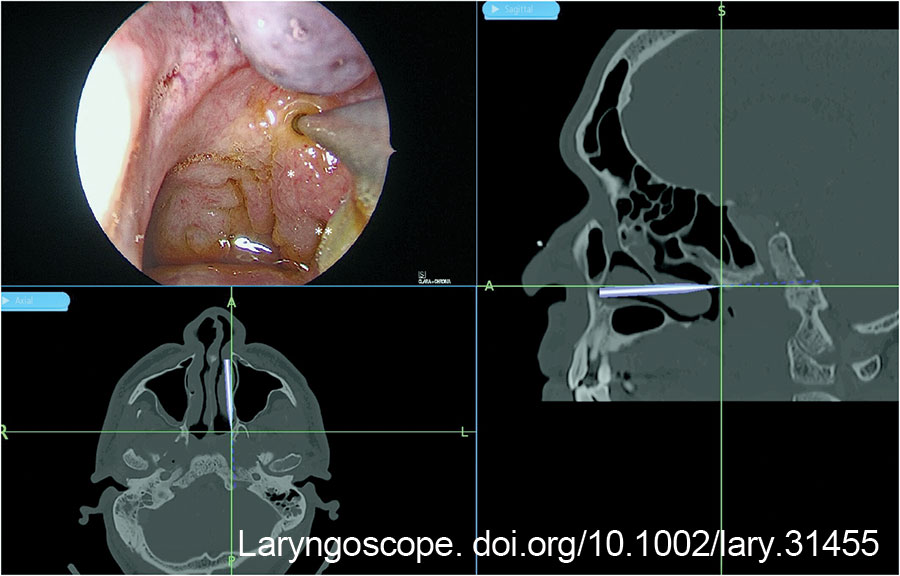
The post-nasal space was examined with a 0-degree Hopkins rod, and the site of the abscess was checked against the image guidance system (Fig. 1). A superficial mucosa biopsy was first performed to exclude nasopharyngeal carcinoma. The biopsy site also served as a marker for the planned incision. A Megadyne 0016 M 6-inch insulated needle point electrode (Ethicon Inc, Cincinnati, Ohio) was used to create a vertical incision medial to the fossa of Rosenmüller, from the roof of the nasopharynx to the level of the Eustachian tube. A vertical incision was preferred over a horizontal incision to avoid lateral dissection toward the Eustachian tube and carotid artery. The salpingopharyngeus muscle served as the lateral landmark to avoid injuring the Eustachian tube orifice (Figure 1).
Hemostasis of surface mucosal bleeding was achieved with adrenaline-soaked patties and suction diathermy to ensure good visualization before deeper dissection. Dissection was deepened with a combination of electrocautery dissection and blunt dissection with a Freer elevator, 8 mm suction, and Blakesley forceps. Constant awareness of the depth of dissection was important to prevent inadvertent injury to the carotid artery. This was achieved by measuring the tip length of the instruments as a gauge of depth, and frequent checks against the image guidance system.
At a depth of 1.3 cm from the mucosal surface, minimal amounts of turbid fluid were encountered posterior–laterally. Blunt dissection was continued toward the source of the turbid fluid till a pocket with necrotic tissue (Fig. 2) was encountered. The necrotic tissue was removed and sent for histological examination and bacteria cultures. The wound was packed with NasoPore (Stryker, Portage, Mich.), which was removed in clinic one week later. The patient was instructed for regular nasal douche.
Aerobic cultures taken from necrotic tissue grew Pseudomonas aeruginosa. Fungal cultures, tuberculosis cultures, and acid-fast bacilli smears were negative. Histology from the superficial biopsy showed mucosa with lymphoid infiltrates with no granuloma or malignancy. Histology of the deep necrotic tissue showed necrotic collagen with neutrophilic aggregates and encrusted bacteria on the surface, with no mucosa or epithelial cells seen. Fluid cultures from the tympanocentesis grew scant Staphylococcus aureus, which was suspected to be contamination from external auditory canal skin flora.
Post-operatively, the patient was kept inpatient for a week of intravenous antibiotic treatment with meropenem, followed by six weeks of oral ciprofloxacin and co-trimoxazole based on antimicrobial culture sensitivities.
CONCLUSION
This study showcases a safe technique for transnasal endoscopic drainage of upper parapharyngeal abscesses. Pre-operative imaging and planning are important to appreciate the relationship to the carotid artery, while intra-operative image guidance and measurement allow the surgeon to maintain anatomical orientation. Taken together, this technique offers effective and safe access for upper parapharyngeal abscess drainage with minimal morbidity and good cosmesis.