INTRODUCTION
The pericranial flap is a strong, elastic tissue with a large surface that is useful for several indications, including skull base reconstruction after craniofacial resection. It has been the workhorse for anterior skull base reconstruction for decades (Laryngoscope. 1990;100:607-614).
Explore This Issue
August 2021Traditionally, the pericranial flap is raised through the bicoronal scalp incision used for craniotomy, across which it is passed to cover the endocranial side of the defect (see supporting video). Several modifications have been made to adapt its use to endoscopic craniofacial resection. Instead of placing the flap endocranially, it is placed covering the external surface of the defect into the nasal cavity. Osteotomy is performed on the anterior wall of the frontal sinus to transpose the flap through it. Nevertheless, the need to make a bicoronal incision only to raise the flap remains its main drawback.
To address this problem, different endoscopic techniques have been described (Laryngoscope. 2009;119:13-18; Laryngoscope. 2017;127:2721-2724). However, all of these approaches require a skin incision over the glabella to perform osteotomy on the anterior wall of the frontal sinus. Hence, we must choose between a bicoronal or a visible glabellar incision.
We developed a technique to harvest the pericranial flap endoscopically using a single 3-cm incision hidden in the scalp (see Figure 1). Furthermore, we verified that through this endoscopic approach, glabellar incision can be avoided by performing frontal osteotomy endoscopically.
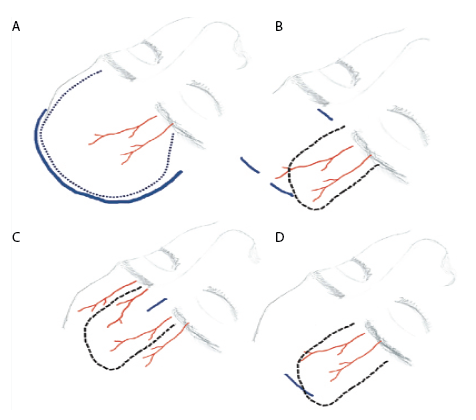
Figure 1. The pericranial flap evolution. A) Bicoronal incision. B) Zanation approach, performing two incisions in the scalp and one in the glabella. C) Single-port approach, through a unique incision in the glabella. D) Single port hidden in the scalp, avoiding any visible scar.
García-Fernández A, et al. Laryngoscope. doi:10.1002/lary.29407
METHOD
First, two cadavers prepared using the Thiel technique were dissected to assess the feasibility of performing osteotomy from within the frontal sinus, as well as the possibility of completing it endoscopically from the outside if necessary. In both cases, modified endoscopic Lothrop procedure (MELP) was performed, and, using a 70° bur mounted on a Straightshot M5 Microdebrider, osteotomy was completed from within the anterior wall of the frontal sinus to expose 2 cm of the periosteum.
Next, this technique was applied in four patients for skull base reconstruction after endoscopic craniofacial resection for malignant neoplasms of the nose. In all cases, MELP was performed prior to craniofacial resection. The frontal sinus floor was drilled out until the anterior wall of the frontal sinus was reached, where osteotomy was performed endoscopically with a 70° bur until approximately 2 cm of the periosteum was exposed. The entire frontal region was then infiltrated with serum and epinephrine at a dilution of 1/100,000. The estimated trajectories of the supraorbital and supratrochlear pedicles were drawn on the left side, and a flap based on both pedicles, approximately 11 cm long and 6 cm wide, was designed. The distal margin of the flap was placed 3 cm posterior to the planned incision, located along an imaginary coronal line passing through the external auditory canal. A 3-cm midline coronal incision was made 1.5 cm posterior to the hairline, and a subgaleal pocket was dissected both anterior and posterior to the incision under direct view. Next, using a 30° endoscope oriented toward the skull and mounted on an optical dissector equipped with a distal spatula and suction channel, the previously created pocket was extended downward until it reached 1 cm above the supraorbital arch laterally and the nasion in the midline.