INTRODUCTION
With the combination of the endoscope, illumination, and a powered instrument, along with the use of a nasal mucoperiosteum flap, the ostium patency rate of endoscopic dacryocystorhinostomy (eDCR) is currently comparable to that of an external approach. Meanwhile, due to its avoidance of a facial scar, better accuracy in the location of the lacrimal sac, and decreased blood loss, eDCR has become much more popular. A nasal mucoperiosteal flap is often designed to prevent stenosis and atresia of the newly created ostium in an eDCR. Here we report a superiorly hinged clubhead-shaped nasal flap that showed satisfactory results for ostium preservation and scar reduction.
Explore This Issue
January 2023METHOD
Surgical Technique
All procedures were performed under general anesthesia. To provide sufficient mucosal decongestion and surface anesthesia, the nasal common cavity and middle meatus were packed with cotton pledgets soaked in 1% tetracaine and 4‰ adrenaline for several minutes. Almost all the procedures were performed with the 0° endoscope except for the examination of the surgical field with a 45° endoscope at the end of the operation. Surgical procedures were as described below (also see the supporting video).
Clubhead-shaped nasal mucoperiosteal flap: Using an insulated needle-tip electrocautery bent at a 45° angle, we started the first mucosal incision above the axilla of the middle turbinate and 2 mm below the roof of the nasal cavity. It was extended 8 mm anterior to the axilla of the middle turbinate and then turned downward and 1.5 cm anterior to the attachment of the uncinate process to an area of insertion of the inferior turbinate.
The second incision was started from the axilla of the middle turbinate and coursed downward 2 mm anterior to the attachment of the uncinate process. When the second incision reached where the insertion of the inferior turbinate was, it turned anteriorly to connect with the first incision. A Cottle septum elevator was then used to elevate the mucoperiosteal flap in a subperiosteal plane. After that, the flap, which looked like the head of a golf club, was tucked into the olfactory cleft to keep it out of the operating field. Mucoperiosteum posterior to the second incision was elevated 2 mm posteriorly to facilitate apposition with the following lacrimal flap.
Bone window (Figure 1): The frontal process of the maxilla, axilla of the middle turbinate, and maxillary line were identified. A curved 15° diamond burr was used to thin the frontal process of the maxilla around the region of the maxillary line. The axilla of the middle turbinate and the lacrimal bone were then partially drilled away to fully expose the medial wall of the lacrimal sac. Note that the bone 4 mm above the axilla of the middle turbinate was drilled away to extend the bone window to facilitate further exposure of the fundus of the lacrimal sac. The uncinate process should be reserved as a bony holder of the following lacrimal flap, even if the attachment of the uncinate process was drilled away and the infundibulum or the agger nasi cell was accidentally entered. For the identification of the anterior-most margin of the lacrimal sac, a small patch of periosteum anterior to and continuous with the reddish lacrimal fascia was inevitably exposed.
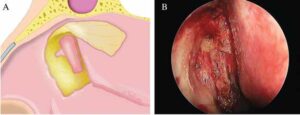
Figure 1. Making the bone window. (A) The bone around the maxillary line was drilled away and the medial wall of the lacrimal sac was exposed. Note the extended area of the bone window, facilitating the location of the anterior edge of the lacrimal sac. (B) Intraoperative view of the bone window and the exposed lacrimal sac.
Posteriorly hinged lacrimal mucoperiosteal flap: The medial wall of the sac was tented with a blunt Bowman’s lacrimal probe through the upper punctum and then incised vertically from the anterior-most margin with a crescent blade. Once the lacrimal sac was opened, the blade was inserted into the sac, and superior and inferior releasing incisions were made to create a posteriorly hinged lacrimal flap. The newly created lacrimal ostium was about 0.5 cm by 1 cm in size.
Placement of two flaps: The lacrimal flap was reflected posteriorly and anastomosed with the mucoperiosteum overlying the bony uncinate process. Subsequently, the clubhead-shaped nasal flap was laid back from the olfactory cleft and repositioned over the bare bone.
Stent insertion (optional): A Crawford stent was inserted through upper and lower canaliculi and retrieved endoscopically. The stent was used in the condition of a severely narrowed lacrimal sac or stenotic canaliculus.
After the operation, small pieces of MeroGel pack were carefully placed into the marsupialized lacrimal sac, into the middle meatus, and over the lacrimal and nasal flaps to keep two flaps in apposition with the uncinate process and anterior edge of the opening of the lacrimal sac, respectively. The bare bone, about 0.5 cm by 1 cm, above the inferior turbinate was initially covered with Surgicel and then followed with MeroGel to facilitate secondary intension healing.
Postoperative Care
Postoperatively, three days of intravenous antibiotics, one week of antibiotic eye drops of tobramycin, and two months of intranasal corticosteroid were prescribed in all eDCRs. Lacrimal irrigation was not routinely performed. Patients were evaluated in terms of anatomical patency and symptom relief one week, three weeks, two months, and six months after surgery with nasal endoscopy. The stent remained in place for three months before being endoscopically removed.
RESULTS
Eight patients with nasolacrimal duct obstruction underwent clubhead-shaped flap eDCRs, all performed by the same surgeon, and were followed up at a mean period of 17.1 months. All patients had the symptom of epiphora except one, who was diagnosed with lacrimal sac mucocele and had only intermittent fullness in the medial canthal area. Surgical success was defined as the resolution of symptoms. Six patients with no stent insertion had relief of symptoms one week after the first nasal endoscopy and those with stent insertion three months after the stent removal. Two patients not living in Beijing were followed up only by telephone as a result of COVID-19. Both were persistently asymptomatic for 21 and 20 months after surgery, respectively. All of the patients had no recurrence and no marked complications.
One interesting finding was that, due to tension-free appositions of nasal and lacrimal flaps, two of the eight rhinostomies were gradually contracted in the anteroposterior direction and finally became fissure-like in appearance two months after the surgery. The fissures, like newly formed Hasner’s valves, separated the lacrimal sac from the nasal common cavity and showed no side effects in tear drainage.