Here are some programs:
Explore This Issue
October 2014ORL Boot Camp
Medstar Georgetown University Hospital
Washington, DC
orlbootcamp.sitel.org
ORL SimFest
Philadelphia, Pa.
uphs.upenn.edu
ORL Essentials Boot Camp
University of Michigan, Ann Arbor, Mich.
orlessentialsbootcamp.com
Annual Neonatology Boot Camp
The Children’s Hospital of Philadelphia
chop.edu
Emergencies in Otolaryngology Bootcamp
London Health Sciences Centre
London, Ontario, Canada
lhsc.on.ca
Find out what’s already available in your institution: One easy way to get started with simulation is to find out what simulation devices and programs are already available at your medical school or hospital. As Dr. Fried explains, at many hospitals, simulation is part of the required training program for anesthesiology residents. Otolaryngology residents could share use of the devices that teach residents how to intubate patients.
“Anesthesiologists are probably the most advanced specialty in terms of simulation. They’ve been doing this for 15-20 years at a very sophisticated level,” he said.
It would also be worth asking around to see if any programs are doing simulations in bronchoscopy, esophagoscopy, or pulmonary and gastrointestinal, he said. You may be surprised by what you never knew was available. “I think if the hospitals that I know of are similar to those in most of the country, there is no sharing of information,” he said.
Join clinical trials: Another inexpensive way to get involved in simulation is to join a clinical trial. Several multicenter trials are underway that aim to demonstrate the efficacy of simulation programs, said Gregory J. Wiet, MD, professor of otolaryngology, pediatrics, and biomedical informatics and program director of the pediatric otolaryngology fellowship at The Ohio State University College of Medicine in Columbus. Dr. Wiet, who is also a member of the AAO-HNS surgical simulation task force, said one of the objectives of the task force is to provide a way for institutions to test the validity and efficacy of simulators that have already been developed. Task force members are currently trying to acquire information on programs being developed and plan to eventually post this information on the academy’s website. The information will make it easier for researchers looking to do multicenter trials. These clinical trials will also eventually be posted on the website.
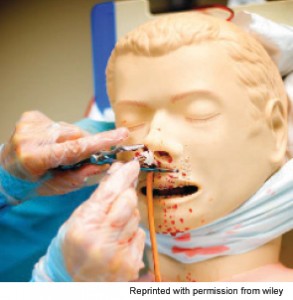
Epistaxis skill station.
Start small: It can be easy to be overwhelmed by the number of simulation options out there. Do you invest in a pricey temporal bone simulator? Change your curriculum? Send all of your residents to ORL boot camps? Dr. Malekzadeh advises focusing on one educational target at a time. “Simulation can seem daunting, as it often requires resources such as space, time, and money. But by focusing on specific procedures residents are struggling with, one can creatively develop simulators to teach the necessary skills,” she said.
Leave a Reply