
© JPC-PROD / SHUTTERSTOCK.COM
One clinical decision that continues to present a challenge to many otolaryngologists is when to order a sleep study for a child in whom obstructive sleep apnea (OSA) or sleep-disordered breathing (SDB) is suspected and for whom an adenotonsillectomy (TA) is indicated.
Explore This Issue
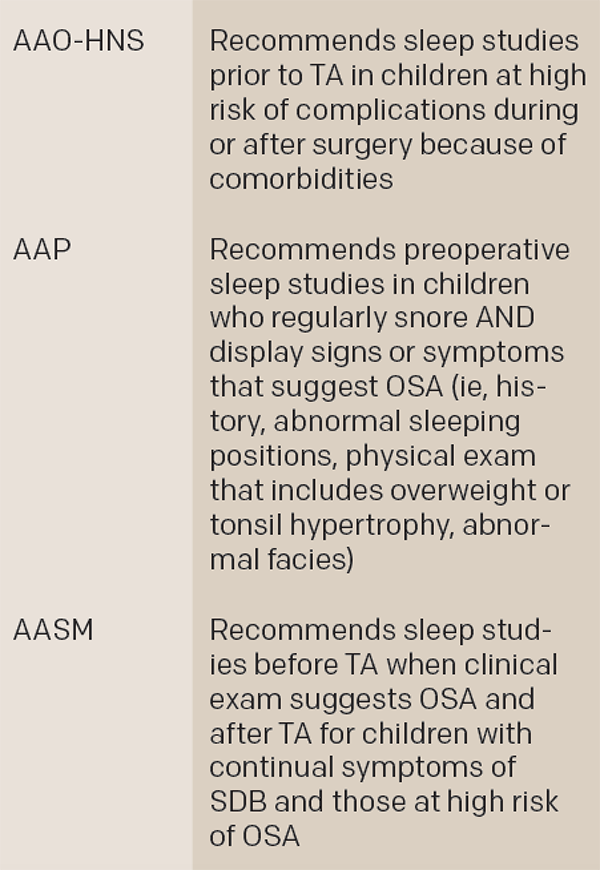
September 2016Clinical guidelines published in 2011 by the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) have provided some guidance on this decision, as have guidelines published in 2012 by the American Academy of Pediatrics (AAP) and, to a lesser extent, those published in 2011 by the American Academy of Sleep Medicine (AASM).
Although all three guidelines contain similar suggestions, they differ significantly in their final recommendations, said Stacey L. Ishman, MD, MPH, surgical director of the Upper Airway Center at Cincinnati Children’s Hospital Medical Center in Ohio, in a recently published article (JAMA Otolaryngol Head Neck Surg. 2016;142:179-118).
In an interview with ENTtoday, Dr. Ishman emphasized that while the AAO-HNS guideline offers the most comprehensive guidance for otolaryngologists, the AAP guideline offers diagnostic options other than sleep studies and recognizes that sleep studies are not feasible in all situations.
Scott Brietzke, MD, MPH, an otolaryngologist at Walter Reed National Military Medical Center in Bethesda, Md., agreed that the AAO-HNS guideline is the most relevant for otolaryngologists and encouraged otolaryngologists to be aware of the other guidelines, while underscoring the need for clinical judgment in determining when and in whom to order a sleep study. “You can’t realistically perform a sleep study with every child who comes through your office door with a sleep complaint,” he said. “You have to balance the benefit of the study and a particular child’s situation.” Informed otolaryngologists, he added, generally use sleep studies judiciously, basing each decision on the patient’s individual situation rather than following a guideline blindly.
A Look at the Guidelines
The recommendations from the AAO-HNS guidelines on the use of polysomnography for SDB prior to TA in children are listed in “AAO-HNS Recommendations for When to Order a Sleep Study Prior to Adenotonsillectomy,” below.
Key Differences among Three Guidelines
TA, adenotonsillectomy; OSA, obstructive sleep apnea; SDB, sleep-disordered breathing
Source: JAMA Otolaryngol Head Neck Surg. 2016;142:179-181
According to Dr. Ishman, the implication of the guideline is that a sleep study is always an option but is not required except in a subset of patients—namely, kids at increased risk for postoperative respiratory complications (see recommendation 1 on complex medical conditions, below).