Subsequently, the surgical microscope and CO2 laser were adjusted and a “Mercedes” incision of the subglottic stenosis was made by CO2 laser. This involves radial incisions to create smooth end transitions from subglottis to trachea. The stenosis was incised over its entire length at approximately 12:00, 4:00, and 8:00 (adjusted to the shape of the stenosis).
Explore This Issue
November 2022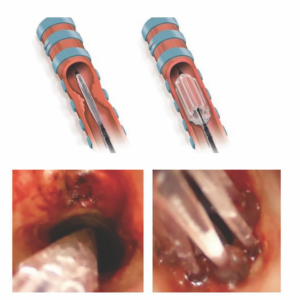
Figure 1. (A) Schematic drawing of Trachealator balloon. Left: deflated, during insertion. Right: inflated. (B) Left: Trachealator
balloon in the subglottic region and trachea before inflation. Right: inflated. The central lumen that can be used for
ventilation and oxygenation now becomes apparent.
After the Mercedes incision, the Trachealator was introduced. The Trachealator is a novel, non-occlusive balloon dilator designed for single use. Depending on its diameter, it is made up of between six and eight separate compartments. When inflated, each compartment exerts a force on the two adjacent compartments, forming a self-contained construction with an open lumen allowing for ventilation and oxygenation by the SSHFJV (Figure 1).
The diameter of the Trachealator balloon was selected according to the expected subglottic diameter for the patient based on age and sex. Each Trachealator balloon has a rated burst pressure of 14 atmospheres regardless of the size. After the Trachealator was inflated, it was held in place for 10 minutes in each patient, and, once deflated, the Trachealator was removed and the procedure was ended. Subsequently, muscle relaxation was antagonized, anesthesia was stopped, and the patients returned to spontaneous breathing.
RESULTS
During CO2 laser incision and dilation with the Trachealator, all patients (13 to 62 years of age) were adequately ventilated and oxygenated by SSHFJV. There were no perioperative or postoperative complications. All patients were examined two to four weeks and three months after surgery.
All patients reported less dyspnea/better breathing after surgery. Although subjective, all patients reported increased exercise tolerance. Two to four weeks after surgery, four out of seven patients reported glottic mucus and the need to scrape their voice. Preoperatively, our patients had a peak flow that measured 45% of their normal rates (normalized for age, gender, and height). Three months post-operation, peak-flow levels had increased to 90% of their normal rates (P < 0.05).