INTRODUCTION
Vestibular schwannoma (VS) is a benign tumor arising from the vestibular portion of the eight cranial nerve, which variably extends into the internal auditory canal (IAC) and the cerebello-pontine angle (CPA). Its management strategies include observation with serial imaging, radiotherapy, and surgery. The modern surgical treatment of VS could range from traditional surgical approaches, which target the tumor from behind (the retrosigmoid and the translabyrinthine approaches) or from above (the middle cranial fossa approach), to the more recent transcanal promontorial approaches, which allow a straight and direct surgical corridor to the IAC and CPA (Otolaryngol Head Neck Surg. 2018;158:710-715; World Neurosurg. 2020;135:e181-e186).
Explore This Issue
March 2023In particular, combining the high magnification and direct visualization of the surgical field provided by the endoscope with the bimanual dissection allowed by the microscope, the expanded transcanal transpromontorial approach (ExpTTA) allows surgeons to treat up to limited Koos stage III VS in a minimally invasive fashion. Tumors up to 3 cm in size with linear progression into the CPA and touching the brainstem can be removed with limited bone drilling and neurovascular manipulation, and no brain retraction (Otolaryngol Head Neck Surg. 2018;158:710-715; World Neurosurg. 2020;135:e181-e186). Indications to ExpTTA are limited to growing acoustic neuromas (as evaluated at magnetic resonance imaging follow-up), with a Koos stage I, II, or III, in patients with severe hearing loss and/or disabling vertigo (Otolaryngol Head Neck Surg. 2018;158:710-715).
Despite the accumulating evidence of feasibility, safety, and positive functional outcomes, the spread of ExpTTA has been restricted to few centers across the world. This could be due to the technical difficulties in using both the endoscope and the microscope in a limited area of exposure, and to the lack of familiarity with the transcanal transpromontorial anatomical perspective.
The aim of this study is to provide a step-by-step description of an ExpTTA for the removal of a Koos II VS. A focus on anatomical details from a transcanal point of view is given, to guide any ear surgeon to master this combined (microscopic and endoscopic) approach.
METHOD
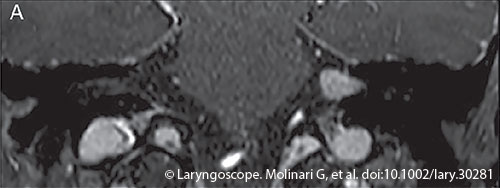
Figure 1. A coronal anterior slice section with T1-weighted high-resolution isotropic volume excitation (THRIVE) sequence, from preoperative magnetic resonance imaging, suspect for Koos II vestibular schwannoma.
We report the case of a 64-year-old female who was referred to our clinic complaining of left nonpulsatile tinnitus and ipsilateral hearing loss of a few years in duration, recently worsened. She also reported sporadic vertiginous episodes. An MRI showed a contrast-enhanced circumscribed mass of 17 × 7 × 7 mm, occupying the left IAC and extending into the most lateral part of the CPA, suggestive for Koos II VS (Figure 1). A CT scan was performed to assess surgically relevant features of the temporal bone, such as the pneumatization of the apex close to the IAC and the height of the jugular bulb, as well as to rule out temporal bone malformations.
Given her auditory function, the dimension and location of the tumor, and the worsening symptoms, she was a candidate for surgical removal of the VS through an ExpTTA.
The equipment consisted of a standard otologic microscope and 14-cm length, 3-mm diameter, 0° and 45° endoscopes, connected to a high-resolution camera system. The patient laid in the supine position under general anesthesia with the head rotated away from the surgeon. Two-channel intraoperative facial nerve monitoring was used throughout the surgery.
After retroauricular incision and creation of the musculoperiosteal flap, the full thickness of the external auditory canal (EAC) was sectioned as close as possible to the tympanic membrane. The remnant EAC was dissected with a periosteal elevator and completely removed after a canalplasty was performed. After excision of the tympanic membrane and removal of the incus and malleus, extensive drilling was performed to enlarge the EAC edges and skeletonize the internal carotid artery region anteriorly, the jugular bulb region inferiorly, and the third tract of the facial nerve posteriorly.
After the endoscopic check of the middle ear anatomy and the relationships with the above-mentioned vascular and nervous landmarks, the dissection kept on with the progressive exposure of the cochlea (from the basal turn to the apex) and the exposure of the vestibule and the spherical recess in the saccular fossa. The IAC dura was exposed from the porus to the fundus of the canal and opened with microscissors to reach the tumor. The access to the IAC through the spherical recess guarantees reach of the area of the facial nerve on a plane behind the vestibular nerves and the tumor. After cautious control of the position of the facial nerve with the neurostimulator, the tumor was removed in a piecemeal fashion. The fundus of the IAC was explored with a 45°-angled optic to complete the removal of the most medial part of the tumor toward the CPA, and to confirm the neural response of the intrameatal portion of the facial nerve at the end of surgery. Finally, abdominal fat was used to obliterate the surgical cavity and the EAC was sealed with a blind sac closure, everting the skin and suturing the cutaneous cylinder with interrupted nonresorbable stitches. An additional layer was obtained by suturing the fibrous-periosteal tissue elevated from the mastoid at the beginning of the operation.
RESULTS
Radical removal of the tumor was accomplished without intraoperative complications in 320 minutes. The patient was extubated at the end of the surgery and no intensive care monitoring was deemed necessary. A postoperative CT scan performed six hours after surgery showed regular postoperative outcomes, highlighting the straight cylindrical surgical route from external to internal auditory canal and CPA. The patient showed grade II facial palsy according to the House-Brackmann scale, which completely recovered with conservative treatment by the three-month follow-up. Postoperative left deafness was confirmed as a consequence of the surgical approach, and the final histologic examination was consistent with VS. The patient was discharged on the eighth postoperative day.