When patients with allergic rhinitis don’t respond to medical therapy, an otolaryngologist’s arsenal of treatment includes surgical options. Among these is radiofrequency (RF) turbinate reduction, also known as RF turbinate ablation or turbinoplasty, an office procedure that advocates say is cost-effective and minimally invasive, with fewer complications than other surgical remedies. Some otolaryngologists, however, are still hesitant to use this relatively new therapy.
Explore This Issue
January 2011Now, a new study takes a look at the long-term results of RF turbinoplasty. The research by Lin and colleagues reports five-year outcomes of RF turbinate surgery, showing that the procedure is both effective and safe for allergic rhinitis patients who are refractory to medical therapy (Arch Otolaryngol Head Neck Surg. 2010;136(9):892-895).
“Although the patient outcome of RF turbinoplasty declines with time, we found that the improvement in symptom scores in the group as a whole was still significant five years after the surgery,” said Hsin-Ching Lin, MD, the study’s first author and an otolaryngologist at the Chang Gung Memorial Hospital-Kaohsiung Medical Center, Kaohsiung, Taiwan. “Our experience has been encouraging overall, and the procedure has become our first surgical treatment choice for allergic rhinitis.”
The retrospective review included 146 patients who underwent RF turbinoplasty during the period lasting from February 2000 to April 2003 at the Chang Gung Memorial Hospital-Kaohsiung Medical Center. The authors found no adverse reactions such as bleeding, infection, recurrent epistaxis, synechiae, nasal dryness, bone necrosis, atrophic rhinitis or olfactory change. A favorable response was defined as improvement of at least one of the common allergic symptoms without worsening of any of the remaining allergic symptoms, along with patient satisfaction with the surgical results. Of the allergic patients, 57.4 percent said they would have the same procedure performed again.
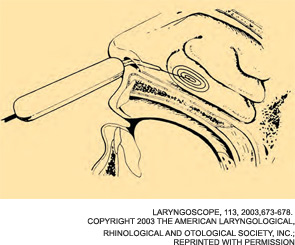
The authors noted in their paper that “because RF is a minimally invasive technique, it does not preclude patients from undergoing secondary laser turbinectomy, submucosal resection of the turbinate, or other traditional procedures.” A previous study by Lin and colleagues followed 108 patients from February 2000 through April 2002 with similar efficacy and safety results (Laryngoscope. 2003;113(4):673-8).
Mixed Reactions
In interviews, otolaryngologists noted some of the limitations of the current study.
In a written comment to ENT Today, Richard Rosenfeld, MD, professor and chairman of otolaryngology at the State University of New York Downstate Medical Center in Brooklyn, N.Y., criticized the design and conduct of the study. He said the data suggested a placebo effect because there was a strong improvement at six months that was reduced substantially at five years. In addition, three of the symptoms that showed significant improvements, sneezing, itchy eyes and itchy nose, would not be influenced by the procedure.
“Turbinoplasty would only be expected to reduce nasal obstruction and, possibly, rhinorrhea,” he noted. Furthermore, “only 57 percent of those who responded to the satisfaction survey said they would have the surgery again (knowing what they know now), which would be expected to be much higher if, indeed, the data in the table reflected improvements.”
Matthew Ryan, MD, assistant professor of otolaryngology at the University of Texas Southwestern Medical Center at Dallas, said the study does not show that RF reduction of the turbinate is now proven to be an effective treatment for allergic rhinitis. And, because the study was uncontrolled, “it is difficult to determine if the clinical improvement noted in the study subjects was due to the RF intervention, other medications and treatments administered through the years, the passage of time or other unknown factors,” he added.
 “Turbinoplasty would only be expected to reduce nasal obstruction and, possibly, rhinorrhea.”
“Turbinoplasty would only be expected to reduce nasal obstruction and, possibly, rhinorrhea.”
—Richard Rosenfeld, MD
Dr. Ryan noted that he isn’t using RF turbinoplasty in his practice, and “I think more people are using different techniques. Compared to other techniques, RF turbinoplasty is not as effective for long-term relief of nasal obstruction.”
Dr. Rosenfeld said that “for allergic rhinitis, in general, this study does not convince me of a benefit. Therefore, I would be more likely to recommend interventions of proven benefit to patients with chronic allergy symptoms [who have been] unresponsive to conventional therapy, such as injection immunotherapy or sublingual immunotherapy, both of which have been shown effective in randomized controlled trials and Cochrane reviews.” Dr. Rosenfeld said he would consider turbinoplasty for patients with allergic rhinitis whose primary complaint is nasal airway obstruction confirmed by nasal endoscopy.
Michael Friedman, MD, professor of otolaryngology-head and neck surgery at Rush University Medical Center and medical director at the Advanced Center for Specialty Care in Chicago, had a different take. “I think the take-home message of the study is that radiofrequency reduction is an option for long-term control of patients who are not responsive to medical therapy,” he said. One of the paper’s authors, Dr. Friedman noted that the study’s purpose was not to compare RF turbinoplasty with other treatments but to determine if RF turbinoplasty has good long-term results. “We as otolaryngologists and physicians treating our patients should have an open mind to multiple options,” he said.
 “I think the take-home message of the study is that radiofrequency reduction is an option for long-term control of patients who are not responsive to medical therapy.”
“I think the take-home message of the study is that radiofrequency reduction is an option for long-term control of patients who are not responsive to medical therapy.”
—Michael Friedman, MD
Dr. Friedman added that more aggressive techniques are not right for every patient. “Sometimes patients are very responsive to medical therapy, and it would be appropriate. However, many patients are reluctant to be on long-term steroids. Although it used to be accepted as having a good safety profile, there is more awareness now of the potential side effects of steroids and other medications.”
While some patients are reluctant to stay on medications for an extended period of time, others don’t respond to steroids or topical medications and don’t want to take systemic medications their whole lives, Dr. Friedman added. “Once we decide to treat the turbinate, the right procedure is determined by the needs of the patient,” he said. “It is not one procedure that is the best procedure. For example, if the patient has a bony turbinate, then RF turbinoplasty would not be the right procedure. A submucousal resection would be a more aggressive procedure giving better results.”
As for other limitations of RF turbinoplasty, Dr. Lin said poor outcomes are possible for patients who have had invasive or nasal turbinate surgeries, a history of radiotherapy for their head and neck cancers, chronic rhinosinusitis with polyposis or the disease of rhinitis medicamentosa caused by extended use of topical decongestants.
Leave a Reply