Stroke, muscular dystrophy, Parkinson’s disease, gastroesophageal reflux disease (GERD), head and neck cancer, Zenker’s diverticulum—each of these disparate conditions can cause dysphagia. As our population ages, more otolaryngologists will be called upon to evaluate patients with dysphagia. In stroke patients, who tend to be older, the prevalence of dysphagia exceeds 50 percent (Cerebrovasc Dis. 2000;10(5):380-386). Undiagnosed and untreated, dysphagia can lead not only to weight loss and failure to thrive, but also to profound social and emotional problems (Ann Otol Rhinol Laryngol. 2008;117(12):919-924).
Explore This Issue
February 2010Patients have no doubt when they have dysphagia, said Katherine Kendall, MD, associate professor of otolaryngology at the University of Minnesota and director of the Lions Voice Clinic at the Minneapolis Veterans Affairs Medical Center. “They come into your office with the complaint,” she said. “The real critical element is figuring out why they have it and what you can do to help them improve their swallowing function.”
To do that, otolaryngologists use a range of diagnostic techniques, including videofluorographic swallow study (also known as a modified barium swallow study [MBS]), flexible endoscopic evaluation of swallowing (FEES) and transnasal esophagoscopy (TNE). ENToday recently spoke with several voice and swallowing disorder experts to discuss the clinical utility of these common diagnostic modalities.
Elicit Complete Information
The first diagnostic tools are a patient’s self-report, the history and the physical examination. Peter C. Belafsky, MD, PhD, associate professor and director of the Voice and Swallowing Center at the University of California at Davis (UC Davis), and colleagues advocate assessing the severity of patients’ symptoms. They have developed and validated a 10-question patient self-report dysphagia-specific outcome survey called the Eating Assessment Tool, or EAT-10. The tool, which is scored by adding patients’ ratings of their symptoms, can help establish initial symptom severity, direct treatment and evaluate therapy and surgical outcomes. An EAT-10 score of three in the setting of mild inflammation on esophagoscopy, for instance, may indicate a mild, non-erosive case of GERD amenable to management with behavioral modifications. A score of 20 indicates that dysphagia is severely affecting the patient’s quality of life and warrants an aggressive team approach for diagnosis and treatment. The tool helps to track outcomes, because it can be quickly administered and scored at each patient visit.
 If you want to stack the deck in the patient’s favor, you need to know as much of the relevant history as you possibly can. A pre-fluoro history and clinical exam is essential.
If you want to stack the deck in the patient’s favor, you need to know as much of the relevant history as you possibly can. A pre-fluoro history and clinical exam is essential.—Rebecca J. Leonard, PhD
Maximizing the MBS
The MBS has become a staple in assessing the safety and effectiveness of oral and pharyngeal swallow. “But if that’s all you’re doing with this study, then you’re underutilizing it,” said Rebecca J. Leonard, PhD, professor of otolaryngology at the UC Davis Medical School and Voice and Swallowing Center. She and her colleagues recommend adhering to a standardized protocol that involves giving a patient exact amounts and consistencies of boluses of barium substances in graduated fashion, a procedure first advocated by Jeri Logemann, PhD, a professor in the departments of Otolaryngology-Head and Neck Surgery and Neurology at Northwestern University who developed the MBS (Otolaryngol Head Neck Surg. 1997;116(3):335-338). Using a standardized protocol allows a uniform means of assessing patients’ responses to treatment or changes over time and “adds greatly to the value of this study,” Dr. Leonard said.
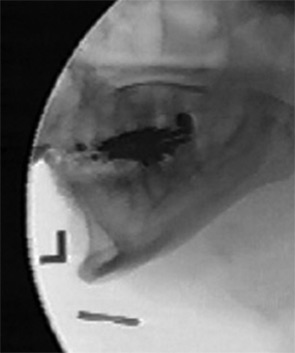
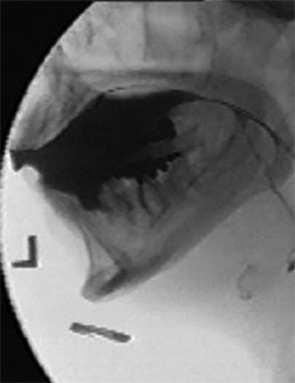
Because any MBS study is a very brief sample of the patient’s swallow function, critical events, such as aspiration, may be missed unless they occur on every swallow. By extracting objective measures of timing and displacement associated with swallowing, the UC Davis Center has been able to develop predictive risk profiles. For instance, using a surrogate measure of pharyngeal strength called the pharyngeal constriction ratio, which is a comparison of the maximally constricted pharynx during a swallow to its fluoroscopic appearance when unconstricted [see Figs. 1 and 2, see p. 16], the team is able to assess a patient’s risk of aspiration even if it is not observed during the study.
Tracking transit time of the bolus through the pharynx and hypopharynx has also allowed useful risk comparisons. A study of patients with acute stroke assessed with MBS showed a strong correlation between prolonged transit—swallows requiring two seconds or more—and readmission with aspiration pneumonia (Arch Phys Med Rehabil.1993;74(9):973-976).
Patients in the intensive care unit or nursing homes, for whom transport to the fluoroscopy suite is not possible, might not be candidates for MBS. It’s also generally avoided in children, for whom exposure to radiation should be minimized.
Keeping Testing In Office
Office-based FEES to assess patients’ oropharyngeal swallow offers portability, avoidance of radiation exposure and real-time visualization of pharyngeal structures. “I find it’s very helpful,” said Robert Stachler, MD, FACS, senior staff physician in the Department of Otolaryngology at Henry Ford Hospital in Detroit. Clinicians can assess patients’ response to positional maneuvers suggested by the speech pathologist and “get automatic feedback on what works and what doesn’t.”
The video “white-out period,” when the pharynx closes, is a minor disadvantage, but Dr. Stachler said clinicians can often infer whether there is aspiration and can look, if need be, to confirm their suspicions before proceeding with a treatment plan.
In addition to its utility as a first test to evaluate swallowing, FEES is also invaluable for monitoring patients after initiation of treatment, said Dinesh K. Chhetri, MD, assistant professor of head and neck surgery and director of the Swallowing Disorders Center at the David Geffen School of Medicine at the University of California, Los Angeles. “You can observe their swallowing and compare the findings to your older video recording,” he said. This allows for recommendations regarding diet and “really gives us a much better handle in taking care of our patients.”
Clinicians who suspect dysfunction in the esophageal phase of deglutition can reduce costs and recovery time by performing TNE in the office setting. Gregory Postma, MD, director of the Center for Voice and Swallowing Disorders at the Medical College of Georgia in Augusta, has been performing TNE for 10 years and reports a nearly 98 percent successful examination rate. TNE is “one of our best tools,” he emphasized.
Because TNE is performed without sedation, it is less expensive and safer than conventional endoscopy (Surg Innov. 2006;13(1):31-39). Its diagnostic accuracy is equal to conventional endoscopy and, in randomized trials comparing the two techniques, patients prefer TNE over endoscopy (Endoscopy 2005;37(6):559-565). TNE can be especially useful, Dr. Postma said, in diagnosing Barrett’s esophagitis and benign and malignant lesions of the esophagus, as well as in follow-up with head and neck cancer patients (Otol Head Neck Surg. 2008;138(4):411-414). Another advantage: Esophageal strictures can be safely treated using balloon dilation in the office.
Selecting Technique
Clinicians must select diagnostic techniques on a “case by case basis,” Dr. Leonard said. For example, if a patient complains of a solid food dysphagia and an esophageal problem is suspected, FEES is not the preferred modality. However, Dr. Belafsky noted, none of these methods is exclusive of the others. “They’re complementary, and in patients with very severe symptoms, a combination of all types might be used at various points in the diagnostic continuum,” he said.
Dr. Leonard also urges clinicians to devote time to a thorough history and to annotate that on patients’ charts. “Sometimes,” she said, “we’re seeing patients for the first time when they show up in the fluoroscopy suite. If you want to stack the deck in the patient’s favor, you need to know as much of the relevant history as you possibly can. A pre-fluoro history and clinical exam is essential.” ENTtoday
Gretchen Henkel is a medical writer based in California.
Top Image Soruce: SPL/PHOTO RESEARCHERS, INC.
Leave a Reply