During the 2017 Triological Society Combined Sections Meeting, held January 18–21 in New Orleans, a panel of experts in head and neck cancer discussed the ramifications of the rise in human papillomavirus (HPV)-positive oropharyngeal cancers. Discussion ranged from the value of HPV positivity in identifying unknown primary tumors to the increasing frequency of difficult family conversations after diagnosis of an HPV-positive cancer to issues that will be faced by more and more survivors.
Explore This Issue
April 2017Christine Gourin, MD, professor of otolaryngology-head and neck surgery at Johns Hopkins University in Baltimore, said that HPV cancers are becoming so much more common that by 2030, it is projected that the most common head and neck mucosal cancer will be HPV-positive oropharyngeal cancer, while the incidence of head and neck cancers arising from other mucosal sites is actually declining. HPV tumors are associated with better survival, as well. “Traditional AJCC [American Joint Committee on Cancer] stage doesn’t seem to apply to that group,” Dr. Gourin said.
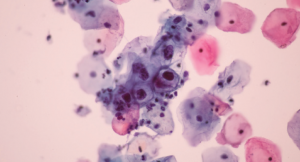
Human papillomavirus.
© Komsan Loonprom / shutterStock.com
David W. Eisele, MD, Andelot professor and director of otolaryngology-head and neck surgery at Johns Hopkins, said that when an adult patient comes in with a solitary neck mass, it is “most likely” going to be cancer, usually squamous cell carcinoma. The earliest diagnostic step shouldn’t be an open-neck biopsy, he said. “Unfortunately, we continue to see patients come in with that procedure having been performed,” he added.
If a nodal metastasis is HPV-related, Dr. Eisele said, it reliably identifies the oropharynx as the site of the primary tumor, often small primaries with advanced nodal disease. HPV status also provides important prognostic information. Pinpointing the primary tumor site improves outcomes, he said.
A 2016 comparison of fine-needle aspiration specimens to resected nodes found that the sensitivity and specificity were “quite good” for linking HPV to the oropharyngeal or the unknown primary patient (J Clin Virol. 2016;85:22–26).
Dr. Eisele emphasized that the presence of p16 protein alone was not a direct marker of high-risk HPV because p16 can be elevated in ways that are not virus-related; histological, anatomic, clinical, and technical factors must be considered.
Dr. Eisele raised concern about proceeding with an initial combination palatine-lingual tonsillectomy approach to identifying the unknown primary, citing studies in which primary tumors were found in the palatine tonsils in many cases, making lingual tonsillectomy, which brings risks for morbidity, unnecessary. (JAMA Otolaryngol Head Neck Surg. 2013;139:1203–1211). Therefore, he said, a sequential approach may be the better choice. Further studies are needed to better define the optimal diagnostic pathway, he concluded.
Treatment De-Intensification
Michael Hinni, MD, an otorhinolaryngologist at the Mayo Clinic in Phoenix, said it’s becoming clear that de-intensifying treatment—using the same intensity of treatment but in a more focused way with less morbidity—is feasible in HPV head and neck oropharyngeal cancers.