The first balloon catheter was approved by the Food and Drug Administration (FDA) for intranasal use in 2005. Since then, at least four other medical devices have received FDA approval for balloon sinus ostial dilation, and balloon sinuplasty rates have increased dramatically. In 2011, the first year a distinct Current Procedural Terminology (CPT) code was available for balloon dilation, stand-alone balloon sinuplasty accounted for 5% of sinus procedures performed on patients with chronic rhinosinusitis. By 2014, that number had risen to 22.5% (Int Forum Allerg Rhinol. 2017;7:600–608). Nationally, the use of balloon dilation increased greater than five-fold, while the use of endo-scopic sinus surgery only increased by 5.9% (Laryngoscope. Published October 8, 2017;doi:10.1002/lary.26941).
Explore This Issue
May 2018The fact that balloon sinuplasty rates increased so dramatically while sinus surgery rates remained stable led to speculation about inappropriate usage. “When you look at balloon dilation usage data, you can see that there are certain hotspots in the country that are doing a vast number of these,” said Nadim Bikhazi, MD, an otolaryngologist in private practice in Ogden, Utah. “One of the concerns has been, is it really being used for the right indications in the right fashion?”
The first-ever clinical consensus statement on balloon dilation of the sinuses aims to ensure patient safety and proper utilization. The document was approved by the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO–HNSF) board of directors and published in February 2018 (Otolaryngol Head Neck Surg. 2018;158:203–214). The statement examines 58 clinical statements regarding patient criteria, perioperative considerations, and outcomes.
“Balloon dilation of the sinuses is an evolving technology that has been shown to have benefit in a number of circumstances,” said James C. Denneny III, MD, executive vice president/CEO of the American Academy of Otolaryngology–Head and Neck Surgery. “As with most evolving technologies in the field of medicine, it’s important to have a blueprint to objectively look at things. Everyone’s end goal is to have a very safe, effective treatment for patients.”
Expected Impact
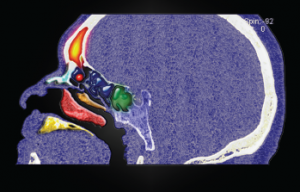
Sinus osteoma.
© Living Art Enterprises / Science Source
According to the consensus statement, balloon dilation is an appropriate treatment for patients who have sinonasal symptoms and positive findings on a CT scan. It can also be used as an adjunct to functional endoscopic sinus surgery (FESS) and may be used in patients who have persistent sinus disease despite previous sinus surgery. There is also a role for balloon sinus dilation in managing patients with recurrent acute sinusitis.