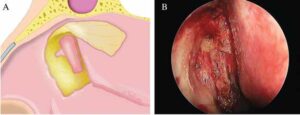
Figure 1. Making the bone window. (A) The bone around the maxillary line was drilled away and the medial wall of the lacrimal sac was exposed. Note the extended area of the bone window, facilitating the location of the anterior edge of the lacrimal sac. (B) Intraoperative view of the bone window and the exposed lacrimal sac.
Posteriorly hinged lacrimal mucoperiosteal flap: The medial wall of the sac was tented with a blunt Bowman’s lacrimal probe through the upper punctum and then incised vertically from the anterior-most margin with a crescent blade. Once the lacrimal sac was opened, the blade was inserted into the sac, and superior and inferior releasing incisions were made to create a posteriorly hinged lacrimal flap. The newly created lacrimal ostium was about 0.5 cm by 1 cm in size.
Explore This Issue
January 2023Placement of two flaps: The lacrimal flap was reflected posteriorly and anastomosed with the mucoperiosteum overlying the bony uncinate process. Subsequently, the clubhead-shaped nasal flap was laid back from the olfactory cleft and repositioned over the bare bone.
Stent insertion (optional): A Crawford stent was inserted through upper and lower canaliculi and retrieved endoscopically. The stent was used in the condition of a severely narrowed lacrimal sac or stenotic canaliculus.
After the operation, small pieces of MeroGel pack were carefully placed into the marsupialized lacrimal sac, into the middle meatus, and over the lacrimal and nasal flaps to keep two flaps in apposition with the uncinate process and anterior edge of the opening of the lacrimal sac, respectively. The bare bone, about 0.5 cm by 1 cm, above the inferior turbinate was initially covered with Surgicel and then followed with MeroGel to facilitate secondary intension healing.
Postoperative Care
Postoperatively, three days of intravenous antibiotics, one week of antibiotic eye drops of tobramycin, and two months of intranasal corticosteroid were prescribed in all eDCRs. Lacrimal irrigation was not routinely performed. Patients were evaluated in terms of anatomical patency and symptom relief one week, three weeks, two months, and six months after surgery with nasal endoscopy. The stent remained in place for three months before being endoscopically removed.
RESULTS
Eight patients with nasolacrimal duct obstruction underwent clubhead-shaped flap eDCRs, all performed by the same surgeon, and were followed up at a mean period of 17.1 months. All patients had the symptom of epiphora except one, who was diagnosed with lacrimal sac mucocele and had only intermittent fullness in the medial canthal area. Surgical success was defined as the resolution of symptoms. Six patients with no stent insertion had relief of symptoms one week after the first nasal endoscopy and those with stent insertion three months after the stent removal. Two patients not living in Beijing were followed up only by telephone as a result of COVID-19. Both were persistently asymptomatic for 21 and 20 months after surgery, respectively. All of the patients had no recurrence and no marked complications.