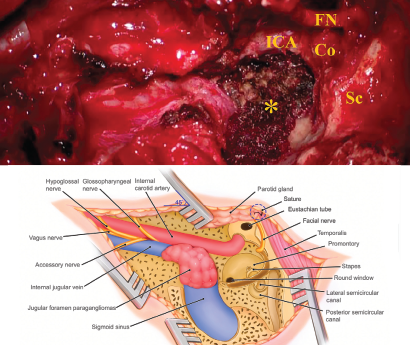
Figure 1. Schematic illustration of the infratemporal fossa type A approach (IFTA-A) with tension-free anterior rerouting of the FN. A) This intraoperative photograph shows the surgical field around jugular foramen after removing the jugular foramen paragangliomas with the modified surgical procedures. B) This illustration demonstrates anatomic structures around the jugular foramen following tension-free anterior rerouting of the facial nerve. Co = cochlea; FN = facial nerve; ICA = internal carotid artery; Sc = semicircular canal: * = jugular bulb, while the tumor was removed, and inferior petrous sinus was packed with Surgicel.
Explore This Issue
July 2021© Kong D, et al. Laryngoscope. DOI: 10.1002/lary.29658
The study included 15 women and five men, with a mean age of 49.58 years (range: 24–69 years). Eight (40%) and 12 (60%) patients were diagnosed with Fisch class C2 and C3 tumors, respectively.
GTR was achieved in 19 patients (95%). One patient did not obtain GTR due to extensive intraoperative bleeding and tumor infiltration of the internal carotid artery. Eighteen patients (90%) had an estimated blood loss of 100 to 450 mL (mean: 265 mL). The blood loss in the other two patients was 1,000 mL and 1,200 mL. Overall, the average blood loss was 360 mL, and the mean surgical time was 3.97 hours (range: 2.92–4.75 hours).
The preoperative FN function was HB grade I in all patients. FN function was HB grade I–II in 18 patients (90%) at the last postoperative follow-up. These patients had a positive response to an electrical stimulation of 0.5 mA after tumor removal, while an FN monitor was applied intraoperatively. The remaining two patients showed HB grade III FN function.
Five patients (25%) displayed dysfunction of the preoperative lower cranial nerves (CNs). One patient (5%) experienced newly developed lower CN IX deficit postoperatively. Cerebrospinal fluid leakage occurred in one patient (5%) intraoperatively; this leakage was successfully repaired with a muscle plug and abdominal fat packing. One patient (5%) experienced brain infarction on postoperative day three; this patient recovered completely. There was no other complication associated with surgery. One patient with GTR was recurrent four years postoperatively. The duration of follow-up ranged from 15 to 94 months (mean: 43.35 months).