What will a multi-institutional review of failed free tissue transfer management contribute to establishing a logical, algorithmic, experience-based approach to failed free flap management?
BOTTOM LINE: The recipient site of the initial failed free flap is the most important factor affecting its management and, in many cases, a second free flap in the acute setting is appropriate.
Explore This Issue
March 2021BACKGROUND: Free tissue transfer has become the preferred reconstruction method in patients with head/neck composite defects following oncologic surgery or traumatic loss; however, despite advancements in technology and technique, some flaps still fail. Although algorithms exist to address approaches to initial head and neck reconstruction, literature offering guidance on flap failure remains sparse.
STUDY DESIGN: Retrospective case series.
SETTING: Department of Otolaryngology, Oregon Health and Science University, Portland, Ore.
SYNOPSIS: Researchers conducted a retrospective, multi-institutional chart review to identify patients who suffered total free flap loss during primary hospitalization from 2006 to 2019. A total of 118 patients (69 males, 49 females, mean age 63 years) met study criteria. Patient ages, comorbidities, risk factors, flap characteristics, tumor specifics, and length of hospital stays were analyzed. Types of dead flaps reviewed included osteocutaneous, fasciocutaneous, myocutaneous, muscle only, and bowel. Of all 188 failed flaps, osteocutaneous was the most common (44%). The most common cause of flap failure was an arterial thrombus (40%), followed by venous (22%) and combined arterial/venous (13%). Osteocutaneous flap failures, fasciocutaneous, bowel, and muscle-only flaps were most commonly managed with a second free flap. Authors concluded that although a second free flap is often the preferred treatment, in the acute setting, local or regional flaps may be viable depending on the recipient site, circumstances of flap loss, and patient-specific comorbidities. Recipient site of the initial free flap was the only statistically significant parameter strongly correlated with management. The collected observational data provided adequate insight for authors to create a proposed management algorithm, however (see Fig. 1). Study limitations included the sole use of medical documentation to discern complex surgical decision making.
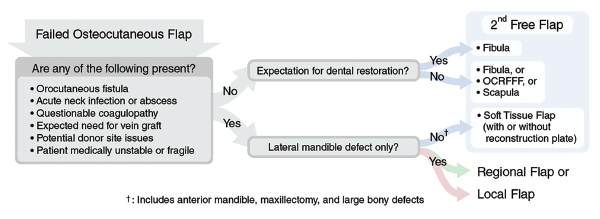
Fig. 1. Proposed algorithm for management of the acute loss of an osteocutaneous free flap to the head and neck. OCRFFF = osteocutaneous radial forearm free flap.
© Source: Laryngoscope. 2021;131:518-524
CITATION: Bender-Heine A, Sweeny L, Curry JM, et al. Management of the acute loss of a free flap to the head and neck—a multi-institutional review. Laryngoscope. 2021;131:518-524.