INTRODUCTION
The differential diagnosis for sphenoid sinus opacification is broad and includes benign, malignant, and infectious etiologies. Patients may present with an atypical headache, retroorbital eye pain, visual disturbances, or sinonasal complaints, or it may be asymptomatic and incidentally noted on imaging for another indication. Generally, persistent sphenoid sinus opacification is evaluated and treated surgically with a sphenoid sinusotomy and biopsy as indicated.
Explore This Issue
February 2023Sphenoid sinus opacification after operative intervention can reoccur due to scarring or bone remodeling and is reported to happen in 10% of cases, a rate that may be even more pronounced in the setting of mucoceles and fungus balls (Int J Surg Case Rep. 2021;79:18-23). The bone remodeling phenomenon has been described in the frontal sinus with restenosis following endoscopic modified Lothrop procedures (Int Forum Allergy Rhinol. 2019;9:1387-1394). Recent studies have found that placement of vascularized flaps or mucosal grafts resulted in reduced rates of stenosis and neo-ossification (Int Forum Allergy Rhinol. 2019;9:1387-1394).
METHOD
Operative Set-up
Patients are prepped and draped in the typical fashion for endoscopic surgery with exposure of the face. Computed tomography image guidance is registered using skin surface matching and is calibrated to within 1 to 2 mm of accuracy. The entire procedure is performed using a 0° endoscope.
Posterior Ethmoidectomy and Sphenoid Sinusotomy
Typically, the dissection is started on the side of the pathology. The inferior and middle turbinates are gently lateralized to improve the space within the nasal cavity and open access to the sphenoethmoidal recess. Any synechiae from prior surgery is carefully divided and the superior turbinate is identified. The location of the sphenoid sinus is confirmed using the computer navigation system, which can be helpful in the setting of severe scarring and bone remodeling. A retrograde posterior ethmoidectomy is performed using Kerrison rongeurs and microdebrider to expose the anterior wall of the sphenoid. Thru-cutting forceps are used to resect the inferior one-third of the superior turbinate. The region of the ostium of the sphenoid sinus is entered and dilated with the Cottle. A Kerrison rongeur is used to enlarge the sphenoidotomy with removal of the anterior wall of the sphenoid sinus superiorly toward the planum and laterally toward the orbit. At this point, purulence, fungal elements, inspissated secretions, or other pathology may be encountered and require culture, biopsy, irrigation, or suctioning.
Vomer-Rostral Flap Design and Elevation
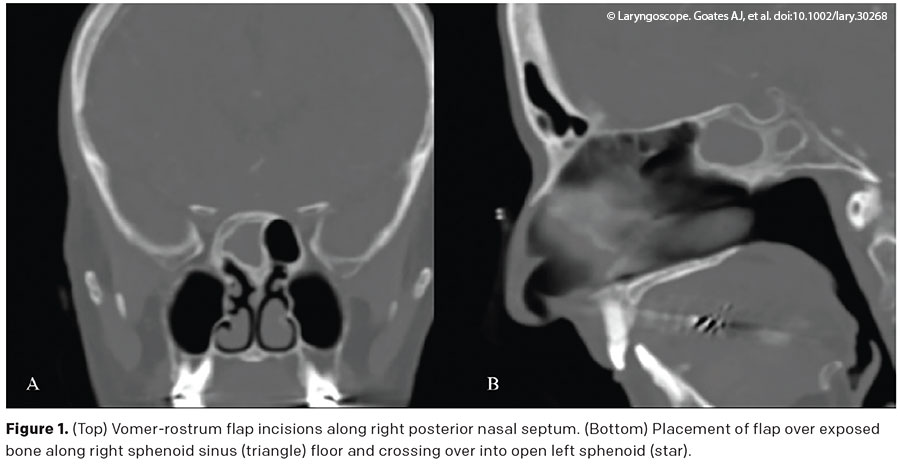
The mucosa over the sphenoid rostrum and nasal septum is elevated to expose the sphenoid rostrum bone. A rescue flap incision is performed with a needle-tip Bovie set at 10 W. This incision is started at the sphenoid sinus ostium and progresses anteriorly along the septal mucosa for about 1 to 2 cm and parallel to the palate. Then, the incision is turned inferiorly at a 90° angle toward the nasal floor, taken to the level of the superior border of the choana. An inferior mucosal incision is performed from the superior arch of the choana and carried anteriorly to join with the anterior incision. Using a Cottle dissector, the mucosal flap from the sphenoid rostrum is elevated with preservation of the vascular pedicle. The mucosal flap along the sphenoid rostrum containing the posterior septal artery is mobilized inferiorly, exposing the underlying bone (see Figure 1).
Rostrum Drilling and Expanding the Sphenoid Opening
A high-speed drill is used to remove the sphenoid rostrum and enlarge the sphenoid sinus opening. An osteotomy is performed inferiorly toward the sphenoid floor and then medially toward the vomer. The contralateral septal mucosa is elevated off the rostrum, and the contralateral sphenoid sinus may be opened if bilateral sphenoidotomy is warranted. The posterior part of the vomer that articulates with the sphenoid rostrum is removed. Then the rostrum is removed. This last step allows wide exposure of the floor of the sphenoid. The inter-sphenoidal septation may be drilled out to ensure communication between both sphenoid sinuses. In case of bilateral sphenoidotomy, the contralateral sphenoid sinus should be widely open, with enlargement of the natural ostium. The vomer-rostrum mucosal flap is then rotated to cover the large area of exposed bone along the inferior border of the sphenoidotomy and sphenoid floor. Frequently, a mometasone-eluting stent is placed, securing the flap in place in contact with all borders of the sphenoidotomy. The absence of bone over the carotid or optic nerve should be considered. In general, a mini stent is used, and the stent should be placed so that it crosses into the sphenoid just beyond the sphenoid face and then protrudes from the sinus, while ensuring that there is no contact in the region of the internal carotid artery or optic nerve. Patients are then dismissed on steroid irrigations until follow-up debridements, which occur generally at one and four weeks (see supplemental video).
RESULTS
This technique has been used on four patients, including two sphenoid sinus fungus balls and two cases of recurrent sphenoiditis. One patient had two prior surgeries for sphenoiditis at another institution with recurrence; they each underwent the described wide sphenoidotomy with rostrum-vomer flap, and at four weeks they had well-healed and widely patent sphenoid sinuses (see Figure 1). All four patients at follow-up had widely patent sphenoid sinuses, with follow-up time ranging from two to six months.