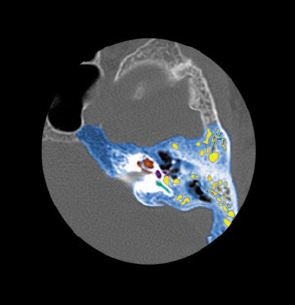
Image Credit: Living Art Enterprises, LLC / Science Source
Temporal bone and inner ear structures.
BOSTON—Hugh Curtin, MD, chief of radiology at Massachusetts Eye and Ear Infirmary in Boston, showed a slide presenting a long list of diagnoses that need to be considered in the case of a common problem, pulsatile tinnitus: Aberrant carotid, a glomus, arteriovenous fistula, pseudotumor cerebri, and arachnoid granulation were included, but the list went on.
Explore This Issue
July 2015While it’s certainly possible to run through all of these potential causes using imaging, it’s not ideal, making information from the ordering physician very useful in tailoring an imaging approach, Dr. Curtin said during a session focused on neuroradiological imaging in otologic disease, held at the Annual Meeting of the Triological Society in April, part of the Combined Otolaryngology Spring Meetings.
“Just a little bit of clinical information can be very helpful to us as radiologists,” he said. “The orders come in: Do you want to do MRV [magnetic resonance venography]? Do you want to do CT, CTA [computed tomography angiography]? What exactly do you want to do? If we know a little bit of the clinical information, it really does help guide us.”
Results of an otoscopy, for instance, are quite useful, he said. “If you have a normal otoscopy, then we’re going to go one way—but if it’s a red mass, CT, to look for these little plates of bone, is the way we tend to start,” he said. “If it’s a normal otoscopy, then we want to know if this is a pseudotumor cerebri candidate. These bits of information can save us a huge amount of time. To rule out everything, we would probably have to have several time slots on the MRI [magnetic resonance imaging], and it becomes a practical consideration.”
For most problems of the temporal bone, he said, imaging is generally started with CT, not MRI. “The only time we really start with MRI is when we’re looking for an acoustic neuroma, and indeed almost everything else is done with CT,” he said.
“The reason our first step is with CT is because we get such good bone detail—CT has very good density differences, contrast, the ability to visualize the small structures. This is really how we’ll evaluate anything that has a thin plate of bone or just a small bony structure that we may want to look at.”
Magnetic resonance is the best imging method when looking at subtle differences in soft tissues, he added, but when it gets up to bone, the resolution of CT is supreme.
He emphasized the importance of oblique imaging. For instance, when looking for dehiscence of the superior canal, radiologists look for the highest bony resolution, he said, and “we try to do images that are perpendicular and parallel to the actual little bit of bone that we’re trying to assess.”
One way MRI is used is in non-echo-planar diffusion-weighted imaging (DWI) in cases of recurrent types of cholesteatoma. The initial evaluation will be done with CT, because of the attention to bone erosions. But non-echo-planar DWI can be useful in assessing potential changes when those images are cross-referenced with others, Dr. Curtin said.
Congenital Hearing Loss
Caroline Robson, MD, chief of neuroradiology at Boston Children’s Hospital, reviewed considerations in imaging of children with congenital hearing loss.
Multi-detector CT, she said, is best for assessing children with external and middle ear anomalies who present with conductor or mixed hearing loss, as well as those suspected of having congenital cholesteatoma. “Both CT and MR provide excellent information regarding the evaluation of children with sensorineural hearing loss, and the choice of the modality is going to depend on several factors,” she said.
CT would probably be best for first-line imaging for a child who could get through the exam easily without sedation but would need sedation or general anesthesia for an MRI exam.
But MRI would be best for a child who is a potential cochlear implant candidate, due to the need for information on the integrity of the membranous labyrinth and the presence and size of or absence of the cochlear nerves. And MRI is definitely best for children with sensorineural hearing loss suspected of having concurrent brain anomalies, she said.
“Whenever possible, we attempt to avoid sedation or general anesthesia,” Dr. Robson said. “The newest generation multi-slice CT units obtain images in a matter of seconds. And so, provided a patient is either asleep or cooperative, many times CT can be obtained without sedation.”
Both CT and MR are conducted, when possible, with children napping, something most successful with infants younger than nine months of age. Motion-reduction sequences and motion-tracking devices are great when imaging the brain but not so useful for the fine detail required when imaging the temporal bone region. “In more cooperative children, we use video goggles and the ministrations of a child-life specialist to encourage us to get through MR without sedation,” Dr. Robson said.
She also touched on the sometimes-difficult subject of what constitutes an enlarged vestibular aqueduct. Based on findings from a Cincinnati group involving a large number of measurements, it’s agreed that the midpoint measurement of a normal vestibular aqueduct should be less than 1 mm, and the opercular measurement should be less than 2 mm.
There are cases that need to be acknowledged where the rule can’t be so rigidly applied. Because the course of the vestibular aqueduct is an oblique one, short-axis reformats should be used in the evaluation, a point made in a study of 15 patients by Dr. Curtin. He and his colleagues determined that, when it is examined in this way, the aqueduct should really measure less than 1 mm along its course. This, Dr. Robson said, “introduces a gray zone, in that patients with a normal midpoint diameter but with an opercular diameter of between 1 to 2 mm could be potentially abnormal.
“Indeed,” she said, “in some of these children we have actually noticed cochlear incomplete partition type 2 anomalies. I think that is the gray zone where we would perhaps provide a measurement rather than coming down hard on saying whether or not it’s enlarged.”
Thomas Collins is a freelance medical writer based in Florida.