Explore This Issue
November 2013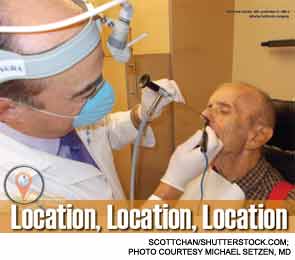
There’s a new development in the surgical management of inferior turbinate hypertrophy (ITH), and, despite medicine’s fascination with the latest technology, it has nothing to do with lasers, radiofrequency ablation, microdebridement or any of the other new medical devices that have dominated the ITH literature.
Indeed, the “buzz” in ITH surgery these days has to do more with the location of surgery rather than with the surgical technique or equipment employed, said Timothy L. Smith, MD, chief of rhinology and sinus-skull base surgery at the Oregon Health and Science University in Portland, and a member of the ENTtoday editorial advisory board.
Specifically, increasing numbers of rhinologists and other otolaryngologists are electing to perform ITH surgery in the office rather than the hospital, and the primary driver of this trend is economic. In uncomplicated cases, where hypertrophy, rather than serious underlying pathology, is the major cause of nasal congestion, “why incur the added costs and hassle of hospitalization?” Dr. Smith said. “Especially in this era of increasing cost containment, I don’t think insurers are going to continue to pay for those added expenses.”
Michael Setzen, MD, the immediate past president of the American Rhinologic Society and practice management coordinator of the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS), is a major proponent of this move to office-based ITH surgery. Dr. Setzen said he has been performing the procedure out of the office for at least a decade, but added that the benefits of such an approach aren’t just economic. Many of the gains, he said, are on the patient side of the equation. “In my office, I can keep them comfortable; it’s much easier to schedule a time for surgery and keep to that schedule; and, perhaps most importantly, in the types of uncomplicated cases we’re really taking about, I can use just a local anesthetic. So they stay alert and awake and go home in great shape.”
That’s not to say, however, that financial considerations are not an important determinant of making a successful switch to office-based ITH surgery, Dr. Setzen stressed. Without a good understanding of the start-up costs involved and the key ways in which in-office vs. hospital-based reimbursement differ, he pointed out, the transition could be a rocky one.
Start-Up Costs
First, the up-front costs should be considered. Those costs will vary based on whether you have an existing sinus surgery practice or are setting up a new office practice. “If you’re just starting out, you will need to purchase endoscopes, which is the building block of doing any sinus surgery, and then you’ll also need video equipment to photograph and record your cases,” Dr. Setzen said. “This is very important for documenting medical need, for getting adequate reimbursement, for liability, etc.” The price tag for that initial investment “is about $50,000, although that of course can vary depending on the size and scope of your practice,” he said.
Leave a Reply