Image Credit: HomeStudio/Shutterstock.com
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record, and they often misunderstand the use of time when selecting visit levels. Sometimes providers may report a lower service level than warranted because they didn’t feel that they spent the required amount of time with the patient; however, the duration of the visit is an ancillary factor and does not control the level of service to be billed unless more than 50% of the face-to-face time (for non-inpatient services) or more than 50% of the floor time (for inpatient services) is spent providing counseling or coordination of care (C/CC).1 In these instances, providers may choose to document only a brief history and exam, or none at all. They should update the medical decision-making based on the discussion.
Explore This Issue
May 2015Duration of Counseling and/or Coordination of Care
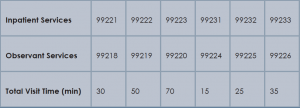
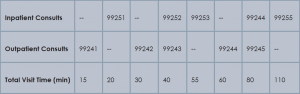
Time is not used for visit level selection if C/CC is minimal (<50%) or absent from the patient encounter. For inpatient services, total visit time is identified as provider face-to-face time (i.e., at the bedside) combined with time spent on the patient’s unit/floor performing services that are directly related to that patient, such as reviewing data, obtaining relevant patient information, and discussing the case with other involved healthcare providers.
Time associated with activities performed in locations other than the patient’s unit/floor (e.g. reviewing current results or images from the physician’s office) is not allowable in calculating the total visit time. Time associated with teaching students/interns is also excluded, because this doesn’t reflect patient care activities. Once the provider documents all services rendered on a given calendar date, the provider selects the visit level that corresponds with the cumulative visit time documented in the chart (see Tables 1 and 2).
Issues Addressed
When counseling and/or coordination of care dominate more than 50% of the time a physician spends with a patient during an evaluation and management (E/M) service, then time may be considered as the controlling factor to qualify the E/M service for a particular level of care.2 The following must be documented in the patient’s medical record in order to report an E/M service based on time:
- The total length of time of the E/M visit;
- Evidence that more than half of the total length of time of the E/M visit was spent in counseling and coordinating of care; and
- The content of the counseling and coordination of care provided during the E/M visit.
History and exam, if performed or updated, should also be documented, along with the patient response or comprehension of information. An acceptable C/CC time entry may be noted as, “Total visit time = 35 minutes; > 50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”