Experts in voice treatment brought their experience to the table in a case-based panel discussion held during the Triological Society Combined Sections Meeting in January 2017, giving insight into their approaches to patient management and injection laryngoplasty.
Explore This Issue
April 2017Transected Recurrent Laryngeal Nerve
© Alila Medical Media / shutterStock.com
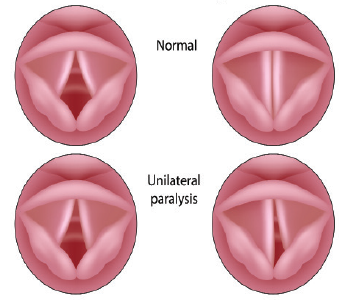
Michael Benninger, MD, chairman of the Head and Neck Institute at Cleveland Clinic, presented a case that involved a 24-year-old woman who had been thrown through a windshield in a car crash. She had developed a “fairly significant” keloid on her neck; she also had a lacerated jugular vein and a carotid artery tear. It was suspected that she had a transected recurrent laryngeal nerve (RLN). Dr. Benninger said that her voice, while “not too bad,” was still something an otolaryngologist would want to help improve.
Panelists Albert Merati, MD, professor of otolaryngology-head and neck surgery at the University of Washington in Seattle, and Karen Kost, MD, FRCSC, associate professor of otolaryngology-head and neck cancer at McGill University in Montréal, said they would likely perform an office injection as their first step.
Robert Sataloff, MD, DMA, FACS, professor and chair of otolaryngology at Drexel University in Philadelphia, suggested a voice assessment. He also suggested that electromyography (EMG) would help determine whether the RLN is really cut and whether reinnervation could be considered. In a 2010 review, some patients thought to have a cut nerve simply had serious injuries with a lot of bleeding and nerves that were crushed by bone but were intact. “I do have a very low threshold for performing EMGs because we have a fair bit of experience being surprised by what we find,” Dr. Sataloff said.
Panelists agreed that the timing of the EMG, in order to get the most reliable results, depends on the details of each case. In this case, Dr. Kost said that at four months she would trust an EMG that showed nothing [no activity], due to the nature of the patient’s injury.
Dr. Benninger noted that this patient received only an office injection, mainly because of her keloid. Her physicians did perform an EMG and found it essentially normal. “She was very concerned about further neck scars,” he added. “We waited, and she did fine…. It looked pretty obvious to everybody that if you get the jugular vein, part of the carotid artery, and the sympathetic trunk, that you probably have gotten the vagus. But in fact, we didn’t.” He noted that the EMG really helped clarify the direction for treatment.
Dr. Merati said the case was more about the virtues of patience than the virtues of EMG. “I would argue that the conclusion shouldn’t be that we should be doing EMGs, but rather that not rushing in to do open surgery is the core of the conclusion,” he said. “If you’re doing augmentation observation, you’re getting to the same place.”
Office Injection Timing
Panelists also discussed timing office injections for patients with vocal fold paralysis. “I love office injections, and I do them pretty much immediately in most people,” Dr. Kost said. “If somebody comes in and doesn’t have any contraindications to an injection, has significant morbidity from their voice, which many patients do—most do, in fact—we have a very, very low threshold for doing an injection to start off with.”
Dr. Merati said he would hesitate in certain cases. “I’m a little hesitant on some of these cases if a patient is going to get framework surgery,” he said. “I don’t love doing framework surgery after there’s been an injection as much as I love doing framework surgery when there’s not been an injection.”
Dr. Sataloff said counseling the patient is important. “I have a long talk with people and tell them that if they’re going to want something definitive, the injection may delay when they can have it,” he said.
The panelists said that they almost never use hydroxylapetite anymore, and most expressed a preference for some form of hyaluronic acid.
They were somewhat split on their use of autologous fat injections. Dr. Benninger said an advantage is that its visco-elastic properties are similar to those of the vocal folds. “The problem with fat is that you have to overinject, and it’s somewhat unpredictable,” he sad. “You get about half the patients where you get a good result and half where you don’t.”
Dr. Kost said her use of fat is fairly uncommon, just because of the convenience of the injectables that are currently available. “I only use fat if patients ask for it, or we do have those patients who come in who just don’t want anything artificial injected in their larynx.”
Dr. Sataloff said the results with fat injections, though not appropriate for all patients, can be long lasting. “It has the potential to be permanent,” he said. “We have people more than 20 years out with one or two injections.”
Thomas Collins is a freelance medical writer based in Florida.
Take-Home Points
- EMG is helpful in determining whether a patient is a candidate for reinnervation.
- In some cases, avoiding a rush to open surgery can lead to the best results.
- Office injections can delay framework surgery.