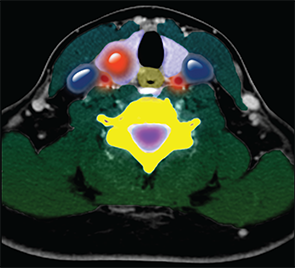
Color-enhanced cross sectional CT image of the neck showing a nodule (large round red density) in the right lobe of the thyroid gland (purple).
Living Art Enterprises, LLC / Science Source
Thyroid nodules are extremely common; some studies using high-resolution ultrasound show that up to 70% of the population have thyroid nodules, with a generally higher prevalence in women and the elderly, said Mark Zafereo, MD, a head and neck surgeon at the University of Texas MD Anderson Cancer Center in Houston.
Explore This Issue
June 2016To assist physicians who are recommending appropriate diagnosis and treatment options, the American Thyroid Association (ATA) released the third iteration of its thyroid nodule and thyroid cancer guidelines in late 2015. The “2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer” are now available from the journal Thyroid (2016;26:1-133).
The guidelines contain 101 separate recommendations for best practices that include diagnosing and managing patients with thyroid nodules and differentiated thyroid cancer, interpreting biopsy results and molecular marker studies, initiating risk assessment and cancer screening, and initiating and monitoring various therapies. Recommendations are rated from strong to weak based on the quality of the evidence available for each.
“There are more options for recommendations now, so you must have the rationale and substantiation for each of those options,” said Ralph P. Tufano, MD, MBA, the Charles W. Cummings MD Professor and director of the division of head and neck endocrine surgery in the department of otolaryngology-head and neck surgery at Johns Hopkins University School of Medicine in Baltimore.
Dr. Zafereo believes that the timing of the update is ideal. “Thyroid cancer incidence in the United States, particularly well-differentiated thyroid cancer, has nearly doubled since the last ATA guidelines were published in 2009,” he said. “Studies have predicted that thyroid cancer may be the third most common cancer diagnosed among women by 2020, with economic impact of $20 billion. Much of this increase is attributable to increased incidental diagnosis of thyroid nodules and cancer on imaging and pathology.”
The Recommendations
Revised guidelines for thyroid nodule management include recommendations on:
- Initial evaluation;
- Clinical and ultrasound criteria for fine-needle aspiration biopsy;
- Interpretation of fine needle aspiration biopsy results;
- Use of molecular markers; and
- Management of benign thyroid nodules.
Revised guidelines for initial thyroid cancer management include recommendations on:
- Screening for thyroid cancer;
- Staging and risk assessment;
- Surgical management;
- Radioiodine remnant ablation and therapy; and
- Thyrotropin suppression therapy using levothyroxine.
Revised guidelines for long-term differentiated thyroid cancer management include recommendations on:
- Surveillance for recurrent disease using imaging and serum thyroglobulin;
- Thyroid hormone therapy;
- Management of recurrent and metastatic disease; and
- Consideration for clinical trials and targeted therapy.
In creating the new version, the guideline panel had complete editorial independence from the ATA. The specific clinical questions addressed in the guidelines were based on prior versions of the guidelines, stakeholder input, and input from task force members; published English-language articles on adult patients were eligible for inclusion.
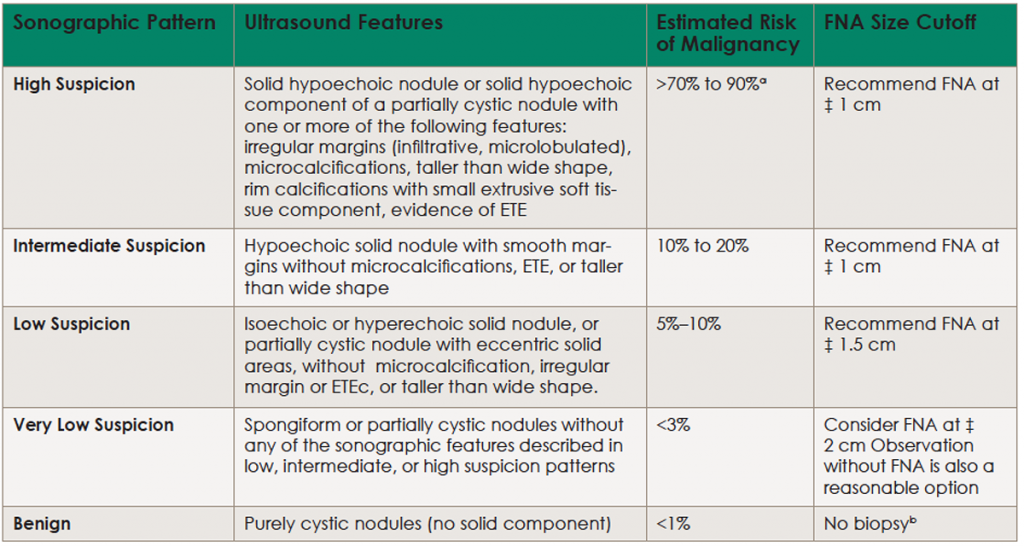
(click for larger image) Table 1. Sonographic Patterns, Estimated Risk of Malignancy, and Fine Needle Aspiration Guidance for Thyroid Nodules
Ultrasound (US)-guided FNA is recommended for cervical lymph nodes that are sonographically suspicious for thyroid cancer.
aEstimate is derived from high volume centers; overall risk of malignancy may be lower given the interobserver variability in sonography.
bAspiration of the cyst may be considered for symptomatic or cosmetic drainage. ETE, extrathyroidal extension.
Updated Information
One reason for the update is that there have been significant scientific advances in evaluation, biopsy criteria and result interpretation, molecular markers, and benign nodule management since the previous guidelines were released in 2009, leading to revised recommendations in all of these areas.
An advantage of these expanded recommendations is a greater ability to fine-tune diagnosis and personalize treatment decisions based on patient preference and clinical context. “With indolent growth pattern and generally excellent prognosis associated with the majority of these cancers, these numbers beg questions about how much diagnostic work-up and treatment is necessary for thyroid nodules and well-differentiated thyroid cancer,” said Dr. Zafereo.
There are rarely sudden shifts in clinical practice, and the ATA guidelines are no exception to that, Dr. Zafereo added. There are some general trends that are more apparent in the 2015 version, however. “These guidelines endorse a generally measured approach to biopsy of thyroid nodules and treatment of differentiated thyroid cancer,” he said. “For example, small and sonographically low-risk nodules may not be recommended for biopsy.”
“It’s certainly been an evolution,” said Dr. Tufano. “The 2015 guidelines are the third iteration, and, each time, there has been a greater attempt to personalize and tailor treatments to individual patients, rather than putting everyone in the same box. Clinicians have to be more thoughtful about what treatment we’re going to render, and the expanded information allows patients to better participate in making the determination of what’s best for them.”
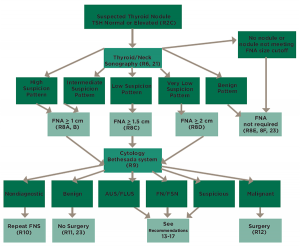
(click for larger image) Figure 1. Algorithm for evaluation and management of patients with thyroid nodules based on US pattern and FNA cytology; several algorithms such as this one are available in the guidelines for quick reference to aid clinicians.
These guidelines can also serve as a starting point for increased dialogue with patients and colleagues about therapy options. “We are seeing a high number of patients with thyroid cancer, and the numbers continue to increase each year,” added Dr. Tufano. “However, the overwhelming majority are small differentiated thyroid cancers; in that circumstance, we feel that since we’re not able to provide objective prognostication on what a tumor will or will not do, we want to make sure we’re very thoughtful about each treatment.”
“There is a general ‘less is more’ trend in terms of surgical management and adjuvant radioactive iodine therapy for low-risk, well-differentiated thyroid cancer,” said Dr. Zafereo. “Ten years ago, many more patients were undergoing total thyroidectomy and postoperative radioactive iodine for well-differentiated thyroid cancer, whereas evidence-based current clinical practice has shifted to more thyroid lobectomies and avoidance of radioactive iodine for smaller well-differentiated thyroid cancers because of excellent long-term outcomes even with lesser therapy.
“Additionally, molecular testing of indeterminate thyroid nodule fine needle aspirates has become much more common over the last decade,” he added, “and the new guidelines outline some general scenarios when molecular testing may be considered.”
Looking Forward
The updated guidelines also include potential areas of interest for future research, including:
- Optimizing molecular markers for diagnosis, prognosis, and therapeutic targets;
- Active surveillance of disseminated tumor cell (DTC)-positive primary tumors;
- Improved risk stratification;
- Improved understanding of the risks and benefits of DTC treatments and optimal implementation/utilization;
- Issues with measurement of Tg and anti-Tg antibodies;
- Management of metastatic cervical adenopathy detected on ultrasound;
- Novel therapies for systemic radioactive iodine (RAI)-refractory disease; and
- Survivorship care.
According to Dr. Zafereo, these recommendations on future research topics are an important step in closing any research gaps. “It’s important as a specialty that we contribute to and stay up to date on the latest evidence in the field of head and neck endocrine surgery,” he said. “This way, we can best educate and care for our patients with thyroid neoplasms, and best communicate and collaborate with our medical endocrinology colleagues.”
“We used to recommend a standard set of treatments,” says Dr. Tufano. “Now, given updated recommendations and the fact that we don’t know the particular behavior of a particular tumor, we should be more thoughtful and complete in our own clinical practices. We want all physicians to sit down and talk about personal care for patients, and how we as physicians can help patients as much as possible without hurting them. These guidelines will prove quite useful in allowing us more flexibility in terms of what care is chosen and how that care is rendered.”
Amy E. Hamaker is a freelance medical writer based in California.