Explore This Issue
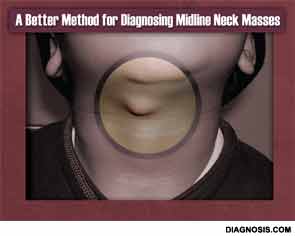
July 2013Knowledge is power, an aphorism usually cited in politics and war, can now be applied to the pre-operative diagnosis of midline neck masses in children. In the largest study of its kind to date, researchers have identified three ultrasound features that have 100 percent positive predictive value (PPV) in predicting the presence of thyroglossal duct cysts (TGDCs) over dermoid cysts—two masses that often mimic each other, complicating pre-operative planning and family counseling.
The research, presented by Dupe Oyewumi, MD, an otolaryngology–head and neck surgery resident at The Hospital for Sick Children, University of Toronto at the 2013 annual meeting of the American Society of Pediatric Otolaryngology held April 25-28 in Arlington, Va., was based on a search of pathology reports from 2005 to 2012 that yielded 91 patients who were confirmed post-operatively to have either a TGDC or midline dermoid cyst (53 were TGCD and 38 were dermoid cysts). For the purposes of the study, ultrasound images that had been obtained pre-operatively were given to two radiologists (clinical fellow Emilio Inarejos, MD, and staff supervisor Mary-Louise Greer, MD, both with The Hospital for Sick Children in Toronto) who were blinded to the pathology results.
The radiologists were then asked to evaluate the images for 14 different features. According to senior author Evan J. Propst, MD, assistant professor in the department of otolaryngology-head and neck surgery at the University of Toronto and associate surgeon at The Hospital for Sick Children, six of those features were found to have high PPV scores for being TGDC:
- presence of a tract (100 percent PPV; P<0.01);
- irregular wall (100 percent; P<0.01);
- ill-defined margin (100 percent; P<0.05);
- internal septae (91 percent; P<0.02);
- intralesional doppler flow (91 percent; P<0.01); and
- solid components (81 percent; P<0.001).
Having a near-certain pre-operative diagnosis for a midline mass yields multiple benefits, Dr. Propst told ENTtoday. Surgery can be scheduled with greater accuracy, for example—a big plus, because removing a TGDC can take up to two hours, versus 30 minutes for a dermoid cyst, he said. Knowing what type of mass is present also makes counseling parents on what to expect and obtaining their consent much easier, he noted.
Moreover, the longer, more extensive surgery for removing a TGDC (Sistrunk procedure) can be avoided in many cases, said Dr. Propst. He explained that because dermoid cysts and TGDCs are often difficult to distinguish, both on ultrasound and pre-operatively based on physical findings, “some surgeons just do a Sistrunk to cover the bases.” The justification, he noted, is that such an approach will reduce the rate of recurrent disease. “Even if they are fairly certain that it’s a dermoid, some surgeons will still do a Sistrunk because they don’t want to see the mass recur.”
Leave a Reply