The real things people need after a disaster often involve physical work or base-level first aid. It was amazing after Katrina how many super-subspecialists signed up to do time in neighborhood clinics, just to help where they could. —Daniel W. Nuss, MD
Explore This Issue
November 2020
In the rush to rebuild vital structures and systems, the need to address a disaster’s impact on staff morale and emotional well-being might be overlooked. After Katrina, Ochsner Health provided emotional support resources and daycare for children, and also “made sure that people got their hours,” said Dr. Carter. “You focus on the people first, and the other stuff falls in line.”
Billion-Dollar Disasters
Although we’re better at predicting disasters, climate-related events are growing. A trend analysis shows that, as of July 8, 2020 is the sixth consecutive year in which 10 or more weather and climate disasters in the U.S. have caused losses in excess of $1 billion.
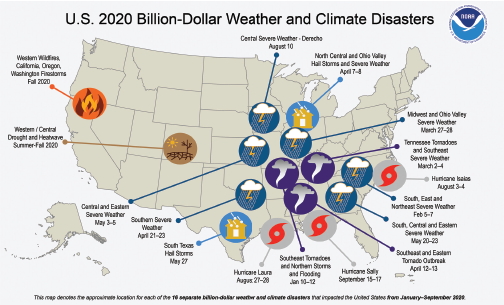
Source: National Centers for Environmental Information, National Oceanic and Atmospheric Administration,
https://www.ncdc.noaa.gov/billions/
Health providers may be especially susceptible to disaster-related psychological stress. “The effects of isolation and inability to work at capacity can be extremely challenging, especially for a group of people who are used to being highly efficient and busy,” said Dr. Walvekar. “The best way to address these issues is to recognize them and face them together. During the worst months of the COVID crisis here, our group met regularly to discuss clinical, individual, and group challenges. Under the right leadership, a disaster experience can help rally faculty and residents to a common goal and vision, which is vital to staying positive and focused.”
Surviving a disaster is a humbling experience for anyone, regardless of their professional status. “No matter what you do for a living, the real things people need after a disaster often involve physical work or base-level first aid,” said Dr. Nuss, who is an otolaryngologist, a skull base surgeon, and a surgical oncologist. “These aren’t glamorous things in medicine, but they need to be done. It was amazing after Katrina how many super-subspecialists signed up to do time in neighborhood clinics, just to help where they could. It reinforces why we should be generous with our time and talents when people are in need, and even as specialists, we should always stay current on the basics of general medicine. That’s one of the lessons.”
Linda Kossoff is a medical freelance writer in Woodland Hills, Calif.
Business Continuity Plans
According to disaster experts, having a plan in place to get your business through the first 72 hours after a disaster occurs is vital. If you have your own practice, consider these steps in creating your own plan.