This “parachute” placement can be used with both autologous free grafts and synthetic materials.
Explore This Issue
December 2020
The parachute technique allows the use of both fascia lata and synthetic materials. We present here a skull base reconstruction of a 1.5-cm defect of the planum sphenoidale.
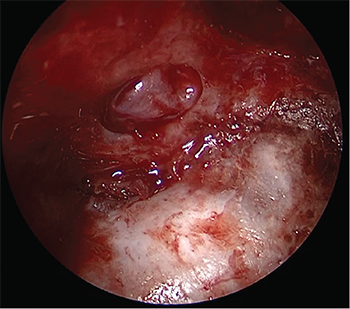
Final view of the two-layer reconstruction using the “parachute” technique.
A Biodesign duraplasty graft (Cook Biotech, West Lafayette, Ind.) in a size that was approximatively 30% larger was designed. A nonabsorbable polypropylene suture (3/0) is passed through the graft near the center in a U shape. The two strands must be long enough to easily exit the nose. Then, the graft is placed in the subdural space using classic microsurgical instruments (angled endonasal blunt hook and seeker, spoon curettes, blunt angled elevators). A slight tension on the strands allows centering the graft on the defect, and then it is applied against the dura without any pucker—hence the name “parachute technique.” It should be noted that the role of the suture is not to anchor the graft but to center it on the defect. The graft is then covered with fibrin glue to seal the reconstruction and the suture is removed, with back pressure being maintained on the graft with a blunt instrument to avoid displacement. Fibrin glue sealing should be used sparingly between the two reconstruction layers to avoid dead space during resorption.
Then, a second graft designed like the first graft is placed in the extradural space, as a “sandwich” to maintain the dura between two graft layers. At the end of the procedure, fibrin glue sealant is applied. With this parachute closure technique, it is possible to associate a multilayer reconstruction using a mucosal graft or mucosal flaps to cover the graft and surrounding bone. We did not use any nasal packing or postoperative antibiotics.
Patients must follow common postoperative advice such as avoiding straining and Valsalva-like maneuvers. Acetazolamide was prescribed only in case of suspicion of intracranial hypertension. We did not use any lumbar drain.
Results
Sixteen patients were included in the study from 2005 to the present. All patients were operated on by the same surgeon.
Iatrogenic CSF leaks were addressed by other centers and then closed during another surgical procedure. The mean postoperative follow-up was 24 months (range = 1–101 months). We did not notice any leak recurrence.