Explore This Issue
November 2013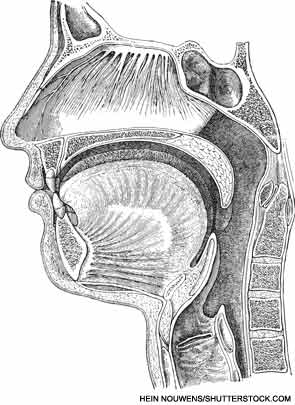
VANCOUVER—Many surgical options exist for obstructive sleep apnea (OSA) patients, but choosing among them can be difficult. Anatomical considerations and available research studies can help guide the decision when it comes to navigating through the many palate surgery procedures, said a panel of experts here at the 2013 AAO-HNS Annual Meeting. Many of the experts who spoke during the mini-seminar on the topic actually pioneered the procedures they discussed.
“I have my own approach to selecting a palate surgery technique for a certain patient, and other surgeons ask me all the time how I make those decisions,” said moderator Eric J. Kezirian, MD, MPH, director of sleep surgery in the Keck School of Medicine at the University of Southern California San Francisco. “I thought we should bring together the surgeons who have developed these procedures or performed research in the area to share their experiences.”
Uvulopalatopharyngoplasty (UPPP): This procedure, the most commonly performed procedure for sleep apnea, has been proven to show improvements in sleep study results such as the apnea-hypopnea index, mortality and quality of life, said Edward Weaver, MD, MPH, chief of sleep surgery and director of outcomes research in the department of otolaryngology-head and neck surgery at the University of Washington in Seattle. However, response rates are sometimes considered less than desirable.
Relocation pharyngoplasty: Hsueh-Yu Li, MD, chief of the department of otolaryngology at Chang Gung Memorial Hospital in Taiwan, developed relocation pharyngoplasty, a procedure that involves removing supratonsillar fat tissue while leaving muscle tissue intact.
Lateral pharyngoplasty: Lateral pharyngoplasty is designed to prevent lateral pharyngeal wall collapse in obstructive sleep apnea, and a primary component for patient selection is sagittal collapse during Mueller’s maneuver. The procedure has been found to improve snoring, sleepiness and apnea. Patients with markedly enlarged tonsils and positional sleep apnea do better with lateral pharyngoplasty, said Dr. Li.
In expansion sphincter pharyngoplasty, the lateral pharyngeal walls are stiffened to prevent their collapse, said Kenny Pang, MD, director and consultant at the Asia Sleep Centre in Singapore. In 2007, Dr. Pang published a randomized trial comparing the procedure with UPPP in patients with mild to moderate OSA who had undergone an examination suggesting palatal collapse without markedly enlarged tonsils (Otolaryngol Head Neck Surg. 2007;137:110-114). The success rate was 78 percent for expansion sphincter pharyngoplasty (ESP) and 46 percent for UPPP, and there was a greater improvement in the apnea-hypopnea index in the ESP group.
Leave a Reply