Background
Obstructive sleep apnea (OSA) is a prevalent disorder and well-established risk factor for cardiovascular disease, myocardial infarction, stroke, and increased mortality. Although continuous positive airway pressure is considered the gold-standard treatment, long-term adherence is unsustainable for many patients. As a result, these patients often seek surgical treatment for their condition. Uvulopalatopharyngoplasty (UPPP) has been offered as a treatment option for OSA since it was first pioneered by Dr. Fujita in 1981. Our purpose is to review the evidence for UPPP in OSA.
Explore This Issue
January 2018Best Practice
There is level 1 evidence that suggests UPPP surgery is an effective treatment for OSA in the appropriately selected patient. It is recommended that an anatomy-based staging system be used in place of a severity-based staging system to predict surgical success. Patients with lower anatomy-based stages consistently demonstrate the greatest likelihood of success with UPPP alone (Laryngoscope. 2017;127:2201–2202).
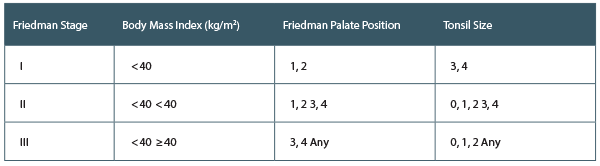
Friedman’s Anatomy-Based Staging System
In 2002, Friedman et al. conducted a retrospective analysis of 134 patients who underwent UPPP for treatment of OSA to validate an anatomy-based staging system (Otolaryngol Head Neck Surg. 2002;127:13–21). Patients were staged based on their Friedman palate position, tonsil size, and body mass index (BMI). Success rates for Friedman stages I, II, and III were 80.6%, 37.9%, and 8.1%, respectively. The authors found their staging system to be an effective predictor of UPPP success. They also proposed that UPPP was effective for stage I patients but counseled against UPPP alone in stage III patients.