A Question of Collaboration
Working within a sleep clinic, otolaryngologists have the opportunity to contribute their expertise in a multidisciplinary setting. “The team at a center for sleep-disordered breathing typically includes neurology, pulmonology, oral and maxillofacial surgery, otolaryngology, and a sleep hygienist (sleep psychologist),” explained Dr. Takashima. “Having a robust center enables the trial of various treatment modalities specifically suited to the patient. For example, if the sleep disorder is more positional and verified by drug-induced sleep endoscopy [DISE], a dental appliance may be appropriate. Or the sleep disturbance can be more anxiety-related, which would be better treated by the sleep psychologist.”
Explore This Issue
December 2020
Because sleep medicine is a newer, evolving field, there’s a need for more sleep physicians of diverse training backgrounds to provide quality care and high-level research, and improve outcomes. —Christine H. Heubi, MD
The potential for collaboration in the sleep arena extends far beyond the sleep centers themselves. Practitioners from different fields who have gone through sleep medicine training share a common experience that helps lay the groundwork for working together. “I find my interactions with sleep colleagues in other disciplines to be incredibly rewarding,” said Dr. Heubi, who collaborates with a team at CCHMC’s Upper Airway Center to manage and treat complex sleep disorders. “Each of us brings a different spin or perspective that would be lost if we all had the same background. It truly is the interplay between each of our disciplines that allows us to successfully manage our patients. Because sleep medicine is a newer, evolving field, there’s a need for more sleep physicians of diverse training backgrounds to provide quality care and high-level research, and improve outcomes.”
The collaborative process plays out in various ways. For example, Dr. Wardrop said that the management of patients with the hypoglossal nerve implant involves a multidisciplinary team, and that the evaluation and management of sleep-disordered breathing in pediatrics is often completed by otolaryngologists.
Patient referrals are also a collaborative byproduct of the sleep specialty. “Referring physicians are aware of my interest in OSA, and they appreciate the extra training that went into obtaining board certification,” said Dr. Takashima. “They’re happy that we as otolaryngologists aren’t just recommending UPPP on all of the patients they refer to us. Diagnostic tests such as DISE and robotic base-of-tongue resections add more scientific rationale for the surgical treatment we do.”
By all accounts, however, collaboration among dual-boarded specialists in the field could be much improved. “Overall, the sleep medicine community hasn’t always welcomed otolaryngologists, or a surgical approach to sleep apnea,” said Dr. Wardrop.
Dr. Woodson agreed. “Collaboration seems to be on a case-by-case basis,” he said. “We do collaborate very well with a large number of people in these other specialties, but I’d say that globally there’s certainly room for a lot more collaboration.”
Board-Certified Sleep Medicine Physicians in the U.S.
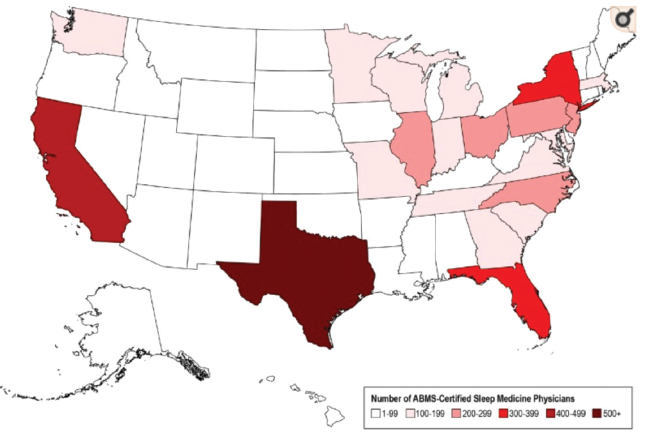
Heat map of the geographic distribution of American Board of Medical Specialties board-certified sleep medicine physicians across the United States.
Original publication in the Journal of Clinical Sleep Medicine; copyright American Academy of Sleep Medicine. Used with permission. https://doi.org/10.5664/jcsm.6406