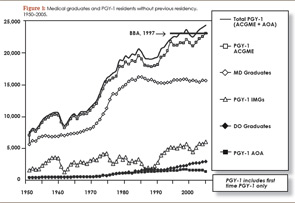
Freezing GME funding at 1996 levels has created a shortage that will be exacerbated as patient demand increases over the next 20 years. Even if 1,000 PGY-1 positions were added annually, the supply-demand gap would persist at least until the year 2050, according to Dr. Cooper [see Figures 1 and 2].
Explore This Issue
January 2010Bring in Mid-Level Providers
Many practices are already hiring physician extenders, primarily nurse practitioners (NP) and physician assistants (PA), who provide general otolaryngologic care in a team-based approach. Dr. Pillsbury warned, however, that current training for ENT NPs and PAs is inadequate, and otolaryngologists who hire physician extenders could be exposing themselves to increased malpractice risk. He and Dr. Kennedy agree that otolaryngologists should take an active role in developing an accredited, university- or AAO-HNS-based certification program for mid-level ENT providers. Dr. Pillsbury sees grants as a possible funding solution.
 Telemedicine provided a way to “increase the availability of care in a situation where we would have had to either turn people away or to create wait environments that would have been clinically unacceptable.”
Telemedicine provided a way to “increase the availability of care in a situation where we would have had to either turn people away or to create wait environments that would have been clinically unacceptable.”—Moises A. Arriaga, MD, MBA, FACS
Revamp Training Programs
Dr. Kennedy believes another solution might be to institute a three-year residency in head and neck medicine, with training in minor surgical procedures, followed by an optional two-year subspecialization. The advantage of this model, similar to one used in Germany, is that those providing primary or secondary otolaryngology care would refer within the specialty for more complicated services.
Some otolaryngologists resist this idea, however. The audience responders at AAO-HNS’s mini-seminar felt that such a move might further fragment the specialty. Dr. Pillsbury sees other problems with reducing the training program. “Funding for training is available for five years or until first certification—and if first certification is only three years, you will have a hard time finding funding for an additional two-year fellowship,” he said.
Develop Telemedicine
In the aftermath of Katrina, neuro-otologist Moises A. Arriaga, MD, MBA, FACS, director of otology-neurotology and professor of otolaryngology and neurosurgery at Louisiana State University in New Orleans, and his colleagues found solutions he believes may be relevant to the impending manpower “storm.”
To maintain their residency program and continue care delivery to outlying areas, his department developed a telemedicine otology program in affiliation with their hospital’s tele-ICU program. With an onsite mid-level provider who manipulated instruments to conduct exams, the program delivered diagnostic services to patients in Baton Rouge for a year. Dr. Arriaga used special teleconference software, a video endoscope, and infra-red video goggles to remotely conduct video endoscopic ear evaluations, cranial nerve examinations, and vestibular assessments. He used Microsoft Word to augment communication with profoundly hearing-impaired patients, who could see his typed communications on a big screen.
Leave a Reply