Explore This Issue
August 2013How to Take Charge of the Future of Sleep Centers
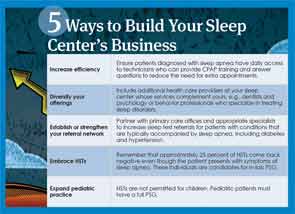
Navigating this new environment requires a dramatic overhaul of the way a sleep center operates. “Centers need to look at their practices and figure out how to be as efficient as they can as they adapt to the new environment of changing reimbursement and patient needs,” said Pell Ann Wardrop, MD, assistant professor of surgery in the division of otolaryngology-head and neck surgery at the University of Kentucky, medical director of the St. Joseph’s Sleep Wellness Center in Lexington and ENTtoday editorial board member. One key way to do this is to facilitate patient access and turnaround time. Have a CPAP technician available every day to see patients who come in for the results of their sleep study and train them on the use of their new equipment. This saves the time and money involved in scheduling an additional appointment to pick up the machine and learn how to operate it.
While streamlining operations, centers should also diversify their services and expand the diagnostic tests and clinical services available at the facility. Hansen suggests that practices incorporate dentists who specialize in treating sleep problems and psychology professionals who offer neurodiagnostic testing and behavioral treatment to attract more referrals and new patients.
Sleep medicine is an integral part of the overall management of many conditions, and this ubiquity provides numerous opportunities for referrals. But, in this new world, centers can no longer wait passively for new patients to materialize. They must take an active role in locating people who need their help.
Partnering with PCP offices is an excellent strategy to broaden a center’s patient base. PCPs can prescribe sleep studies for patients with conditions often accompanied by sleep apnea, including diabetes, arterial fibrillation and snoring. They can refer those at higher risk for sleep apnea, such as individuals who are overweight or who have large necks. Reaching out to PCP offices and reminding them of the value of a sleep study can improve the overall health of these patients, while establishing or increasing a physician’s referral network.
Electronic health records may become an important instrument for increasing PCP referrals. For centers attached to a network that includes a PCP office, EHRs make it easier to screen for patients with health histories that make them candidates for sleep studies and enable easy communication among all the professionals involved in the patients’ care. The depth of information they contain can reduce redundancies in diagnostic testing, providing significant cost savings. They can benefit centers not attached to a network by facilitating smooth and fast information transmission to home care or medical equipment companies. When EHRs are attached to a cloud network, their data can be collected to prove the efficiency and cost-effectiveness of treatment.
Leave a Reply