TORS greatly improves immediate recovery time when compared with traditional open surgery, which frequently requires surgeons to perform a mandibulotomy to access the tumor site. Robotic surgery also prevents some serious long-term quality of life issues. “After chemoradiation,” Dr. Richmon said, “there’s scarring and fibrosis, and patients can experience difficulty swallowing for months and years. TORS allows us to remove the cancer through a minimally invasive approach that translates to very favorable functional outcomes.”
Explore This Issue
April 2014Chemoradiation comes with its own slate of side effects, including mucositis, fibrosis, dysphagia, xerostomia, and tissue necrosis.
Two National Cancer Institute (NCI)-sponsored cooperative working groups are planning prospective clinical trials. Dr. Ferris, who serves on the Eastern Cooperative Oncology working group (ECOG), says that comparing surgical and medical treatments of a class of cancers is an opportunity that shouldn’t be missed. In order to permit direct comparisons of treatments, ECOG trial arms will evaluate deintensification or lowering of radiation doses after transoral surgery. In addition, the treatments will be tested in patients with HPV-positive and HPV-negative oropharyngeal tumors. The transoral surgery can be accomplished with either the daVinci robot or laser microsurgery. In addition to functional outcomes, study objectives will include assessments of feasibility, toxicity, and cost.
Interestingly, the oncologic outcomes of different treatment modalities are not well characterized, said Dr. Richmon. If you compare the survival rates of open surgery, TORS, and chemoradiation, he said, “there’s no high-level evidence supporting one treatment over another at this point. But from a functional standpoint, patients treated with TORS do much better.” And with a younger demographic of patients, long-term side effects have more impact because there are more years of life to interfere with.
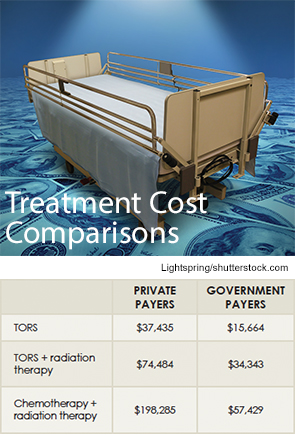
As for cost, TORS is competitive for now. “The machine costs $2 million, but if a hospital utilizes between departments—including urology, otolaryngology, thoracic surgery, cardiovascular surgery, and gynecology—then you spread that cost out,” said Dr. Moore.
Dr. Moore conducted a cost study comparing transoral surgery and standard of care chemotherapy and radiation and found significant cost savings with the surgery (see “Treatment Cost Comparisons,” above).
How the Robot Works
The robot gives the surgeon both an excellent view and articulated robot arm access to those areas just out of sight. Dr. Moore spent a week training at the robot’s manufacturer and then returned to Mayo and started a protocol. Indeed, 50 of his patients underwent the procedure in an off-label use protocol, and those data were combined with that of patients from the University of Alabama at Birmingham and the University of Pennsylvania to submit to the U.S. Food and Drug Administration for approval.
Leave a Reply