For better or worse, medical practices are experiencing change. While many physicians are looking to expand their practice, other physicians are seeking a divorce from their current group.


For better or worse, medical practices are experiencing change. While many physicians are looking to expand their practice, other physicians are seeking a divorce from their current group.

Diana C. Ponsky, MD, assistant professor of otolaryngology-facial plastic and reconstructive surgery at Case Medical Center in Cleveland, Ohio, went to medical school wanting to be a pediatrician. She happened upon otolaryngology “by accident, by scrubbing into a very fascinating cancer case. I was hooked,” she now recalls.
In the more than ten years that Paul Levine, MD, FACS, has served as chair of otolaryngology and head and neck surgery at the University of Virginia in Charlottesville, he has heard his share of complaints about high-powered surgeons who are difficult to work with.
Beyond the handful of long-established and well-integrated sites being labeled as de facto accountable care organizations (ACOs), advocates are seizing the moment and pushing for a bold vision of what role ACOs will play in the movement to reform the health care payment system across the country.

On Feb. 17, 2009, President Obama signed into law the American Recovery and Reinvestment Act of 2009 (commonly referred to as ARRA or the Stimulus Bill) which includes the Health Information Technology for Economic and Clinical Health (HITECH) Act. The HITECH Act includes significant changes to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) that affect otolaryngologists and other health care providers, as well as those who process or work with health care information. Below is a summary of how these new provisions, many of which go into effect this Feb. 17, will affect your practice.
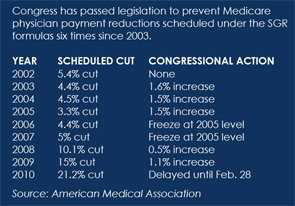
Presdient Obama signed legislationlast month to temporarily prevent a 12.2 percent Medicare payment cut scheduled to take effect Jan. 1. The freeze lasts until Feb. 28, during which Congress is expected to come up with a permanent solution to what some consider a flawed payment system.

How do you plan to deal with workforce shortages? If you are like 55 percent of the audience at an interactive mini-seminar held during the October American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) Foundation annual meeting, you intend to hire additional otolaryngologists to help with practice overload.

SAN DIEGO-Trauma care in the United States is on or heading toward life support. Although this may sound hyperbolic, it points to a need, seen by many otolaryngologists and other surgeons, to raise awareness of the growing gap between the numbers of people in need of trauma services and the accessibility of getting those services.

SAN DIEGO-Hearing aids can become a reliable source of ancillary income for otolaryngologists, according to four speakers in the miniseminar, Hearing Aids: The Dollars and Cents of Dispensing, presented at the annual meeting of the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS).

Patients with cancer of the larynx who are treated at teaching and research hospitals that see high volumes of such patients are the least likely to die within a year of their diagnoses, researchers said at the annual meeting of the American Head and Neck Society.