Otolaryngologists discuss negative pressure redux, combination therapies and airflow-detecting technology in sleep breathing disorders
Otolaryngologists discuss negative pressure redux, combination therapies and airflow-detecting technology in sleep breathing disorders
What is the association between sleep apnea and hypertension in younger patients? Background: Younger patients with sleep apnea have a higher cardiovascular mortality rate compared with their normal counterparts. Because […]
What is the relationship between pre-operative clinical diagnosis of obstructive sleep apnea (OSA) and post-operative hemorrhage? Background: In general, post-operative complications following tonsillectomy are rare, with hemorrhage being one of […]

Awards for the best Triological theses this year went to three researchers, including two co-Mosher Award winners and a Fowler award winner. The awards were given here at the 115th Annual Meeting of the Triological Society on April 20, held as part of the Combined Otolaryngology Spring Meetings.
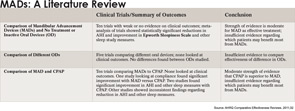
Oral appliances may work better than CPAP for some patients

For otolaryngologists seeing increasing numbers of children with sleep-disordered breathing, whether or not to refer children for a polysomnography (PSG) prior to surgery is not a decision easily made. Currently, only about 10 percent of otolaryngologists request a sleep study in children with sleep-disordered breathing prior to surgery.

The most significant danger to children now is obesity, and of the many related comorbidities that affect obese children, obstructive sleep apnea (OSA) will impact a child’s life more than anything else, according to Carole Marcus, MD, an invited lecturer here last month at SLEEP 2011, the 25th Annual Meeting of the Associated Professional Sleep Societies.Dr. Marcus is a professor of pediatrics at the University of Pennsylvania and director of the sleep center at Children’s Hospital of Philadelphia.

For patients undergoing surgery, identification of known or suspected obstructive sleep apnea (OSA) is critical to avoid or minimize surgical complications that are increased in these patients, experts said here last month at SLEEP 2011, the 25th Annual Meeting of the Associated Professional Sleep Societies.

Among the issues highlighted here last month at SLEEP 2011, the 25th Annual Meeting of the Associated Professional Sleep Societies, was the effect of inadequate sleep on both the health of the individual and on society at large. Two studies presented at the meeting, for example, looked at the effects of inadequate sleep on health care providers and the risks posed to their health and the health of their patients. Another study put into context just how underreported inadequate sleep and sleep disorders are and elaborated on the challenge this poses to otolaryngologists and others who are on the frontlines managing these disorders.
As in all of medicine, the future of sleep medicine will be defined in part by changes evolving under the health care reform law and by the need to slow the unsustainable cost of medical care, experts said here last month at a session at SLEEP 2011, the 25th Annual Meeting of the Associated Professional Sleep Societies,