Presdient Obama signed legislation last month to temporarily prevent a 12.2 percent Medicare payment cut scheduled to take effect Jan. 1. The freeze lasts until Feb. 28, during which Congress is expected to come up with a permanent solution to what some consider a flawed payment system.
Explore This Issue
January 2010On Oct. 30, the Centers for Medicare & Medicaid Services (CMS) issued its final 2010 Medicare physician payment rule. In it, the agency set the payment cut at 21.2 percent using the sustainable growth rate (SGR) formula set forth in federal statute.
The cut would have left physicians with few options, said Ronald B. Kuppersmith, MD, an otolaryngologist in College Station, Texas. “If you’re losing money seeing patients, then you have to either stop seeing those patients or you have to cut costs, which means that employees could lose jobs,” he said.
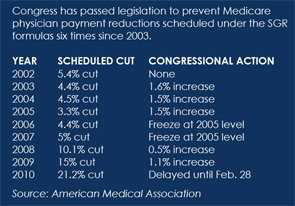
The American Medical Association (AMA) and state and specialty medical societies are pressing for an end to the SGR formula, which began in 1997. Under the formula, the payment update for a year is determined by comparing cumulative actual physician expenditures to cumulative target expenditures in the prior year. If actual spending exceeds the target, payment is cut. The AMA and other physician organizations argue that the methodology for establishing the target spending level does not adequately account for increased spending caused by technological innovation and Medicare benefit expansions. Congress has acted to temporarily prevent the reductions six times since 2003, but it has not changed the baseline for calculating target expenditures. According to AMA materials, “essentially, by temporarily stopping the SGR cuts through the approach of moving the cuts to future years, Congress has created an enormous ‘credit card’ debt that has no hope of being paid off unless the SGR debt burden is eliminated and the physician payment system is rebased.”
—J. James Rohack, MD
Physician have long warned that if the scheduled reduction were to take effect, more physicians would opt out of Medicare and TRICARE, the military health program that has the same payment rate as Medicare. “Access to care and choice of physician for seniors, baby boomers and military families is at serious risk, and Congress must fix the payment formula once and for all this year,” said AMA President J. James Rohack, MD.
House Bill Offers Clean Slate
Physician attempts to dismantle the SGR were set back when House leaders stripped Medicare payment provisions from the health system reform bill before its House passage on Nov. 7, 2009.
Medical groups now are focused on a stand-alone Medicare physician payment reform bill sponsored by Rep. John D. Dingell, D-Mich. The measure is supported by the AMA, the American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS), and more than 100 other physician organizations. It would make the 2010 physician payment update equal to the increase in the Medicare Economic Index, a measure of inflation. That would translate into a 1.2 percent increase.
The bill, H.R. 3961, also would change the baseline on which the payment formula is computed. This would create a clean slate for future payment update calculations, thus wiping away the “debt” caused by the current formula.
The legislation would create two new spending targets, one for evaluation and management and preventive services and the other for all remaining services. The target growth rate for evaluation and management (E&M) and preventive services would be the gross domestic product plus 2 percent, while the target for other services would be GDP plus 1 percent. The change would reduce the likelihood of future physician payment cuts because the target growth rates would be more generous, according to the House Energy and Commerce Committee.
Senate Effort Fails
On the Senate side, a stand-alone Medicare physician payment bill in October failed on a procedural vote. That measure would have repealed the SGR formula and set future Medicare physician payment updates at zero. The legislation, sponsored by Sen. Debbie Stabenow, D-Mich., would have laid “the foundation for establishing a new Medicare physician payment update system through health system reform or other legislation,” according to the AMA.
At press time, Senate Majority Leader Harry Reid, D-Nev., was still working on merging health system reform bills passed earlier this year by the Senate Finance Committee and the Health, Education, Labor and Pensions Committee. The Finance Committee bill contains several Medicare payment provisions that trouble physician organizations. Its 0.5 percent Medicare physician payment increase in 2010 falls short of permanent repeal of the flawed formula.
Another temporary increase would amount to lawmakers kicking the problem down the road again, Dr. Kuppersmith said. A 0.5 percent increase, like the past temporary payment fixes, would not keep up with costs, he said. “It’s still a pay cut because my utility bill goes up. I have to give employees cost of living increases. None of my costs are coming down, and they’re all going up more than 0.5 percent,” said Dr. Kuppersmith, who is president of the AAO-HNS Board of Directors.
The Senate Finance health reform bill also would establish a 10 percent bonus for certain E&M codes for primary care physicians and rural general surgeons that would be funded partly by reducing pay to specialists. On Nov. 4, 20 specialty societies, including the AAO-HNS, sent a letter to Reid outlining their objection to that provision. The letter also voices the groups’ opposition to provisions that would create an independent Medicare commission whose payment recommendations could become law without congressional action, make participation in the Physician Quality Reporting Initiative (PQRI) mandatory, and reduce payment to doctors who are found to have the highest resource utilization.
Although the final CMS Medicare physician payment rule included the bad news of the pending payment cut, it also carried some good news; the agency removed physician-administered drugs from the calculation of the current payment formula. Physicians have no control over the cost of these drugs but get penalized under the SGR as the medications get more expensive, medical organizations argue. The AMA notes that spending on physician-administered drugs has grown at much higher rates than spending for all other physician services. Removal of these drugs from the payment formula will decrease the difference between target and actual physician spending, and thus improve physicians’ reimbursement outlook over the long term, CMS stated. “While this decision will not affect payments for services during calendar year 2010, CMS projects it will have a positive effect on future payment updates,” said Jonathan Blum, director of the agency’s Center for Medicare Management.
The final rule also includes changes to PQRI, a voluntary program under which physicians receive Medicare incentive payments for successfully reporting data on quality measures. The 2010 bonus, which is equal to 2 percent of estimated total allowed charges for covered professional services under Medicare Part B, has been extended to physician groups. Previously, only individual health care providers could report but under the new rule practices with 200 or more eligible professionals would be able to take advantage of the reporting option. This is good news for otolaryngologists; the AAO-HNS notes that the median otolaryngology practice is three physicians. ENTtoday
TOP IMAGE SOURCE: ACARINA/ISTOCK.COM
Leave a Reply